by (Neuro Science School): Evidence for the relationship between gut health and brain health is mounting, with an ever-growing number of studies finding that symptoms of anxiety, depression, and autism can be improved by optimizing gut health…
Here is some of the latest research in this area.
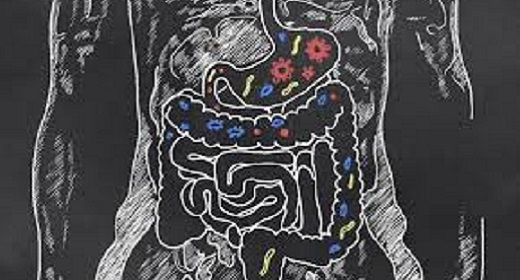
Diet Relieves Anxiety Better than Do Probiotics
Anxiety is a mental disorder that will affect up to 33% of us at least once during our lifetime. In addition, the incidence of anxiety in chronic diseases such as cancer, cardiocerebrovascular disease, and irritable bowel syndrome (IBS), is between 1.4%–70%. The primary intervention for anxiety disorders has been focused on relieving physical symptoms, using psychiatric drugs, and receiving psychotherapy. But there’s a growing interest among researchers in the gut-brain connection, with research showing that the gut microbiota (gut bacteria) “perform important functions in the immune system and metabolism by providing essential inflammatory mediators, nutrients and vitamins. The long-term existence of this immune activation can make brain functions change leading to mental disorders such as anxiety.” And animal studies have found that anxiety can be relieved by changing the gut bacteria.
Researchers from Shanghai Jiao Tong University School of Medicine wanted to answer the question whether improving gut microbiota could relieve anxiety symptoms in humans. They reviewed 21 randomized-controlled studies (the gold standard in research) containing 1,503 human subjects that aimed to treat anxiety by regulating gut microbiota using probiotics and non-probiotic methods such as regulating diet. They found that 5 of the 6 non-probiotic methods (83% effectiveness rate) were better than probiotics (36% effectiveness rate) at relieving symptoms of anxiety.
“One reason that non-probiotic interventions were significantly more effective than probiotic interventions was possibly due to the fact that changing the diet (a diverse energy source) could have more of an impact on gut bacteria growth than introducing specific types of bacteria in a probiotic supplement.”
Two of the studies using non-probiotic methods had participants adopt a low FODMAP diet. FODMAP refers to fermentable oligo-, di-, mono-saccharides and polyols, which are groups of carbs that are notorious for triggering digestive symptoms. Low FODMAP diets are clinically recommended for managing irritable bowel syndrome. Other non-probiotic methods used were eliminating gluten and adding resistant starch (which feeds good gut bacteria).
These results are notable because, as mentioned above, the studies reviewed in this paper were randomized-controlled studies, the gold standard in research. Much of the research on the gut-brain connection in humans has used non-randomized intervention studies and, unlike with randomized-controlled studies, clear causal conclusions can’t be reached with these types of trials.
A Better Diet Can Relieve Depression
A couple of important studies has found that improving the diet can relieve depressive symptoms. These were the first randomized-controlled trials to find that only 3 months on a Mediterranean-style diet reduced depressive symptoms and, in some cases, even resulted in the remission of depression. The important factor seems to be increasing the consumption of nuts and consuming a greater variety of vegetables. I’ve written about one of these studies in an earlier blog.
Gut-Brain Link in Autism
Up to 90% of people with autism also suffer from gut problems. Scientists from RMIT University have now found a gut-brain link in autism. “The [new] study reveals a gene mutation that affects neuron communication in the brain … also causes dysfunction in the gut.”
“They researchers found that this mutation affects:
- gut contractions
- the number of neurons in the small intestine
- the speed that food moves through the small intestine
- responses to a critical neurotransmitter (GABA) important in autism (well known in the brain but not previously identified to play any major role in the gut).”
The next step is to investigate whether tweaking gut microbes could improve mood and behaviour in autism. And I, for one, am optimistic.
As coaches, we often see clients with sub-clinical anxiety or depression. I think it’s imperative that we ask our clients about the quality of their diets and encourage them to eat healthy food. Not to do so is doing them a disservice and can even hinder the process of change. That’s because we can’t have a healthy mind without a healthy body.