by Sarah Richards: Vaccine makers are already planning boosters to attack new versions of the coronavirus, while researchers work to figure out how dangerous they really are…
Dramatic spikes in COVID-19 infection rates over the past year are most often linked to people ditching their masks or gathering in large groups. But infectious disease specialists are increasingly convinced there was another factor at play: The coronavirus itself was changing and becoming easier to spread.
A growing body of genetic sequencing evidence reveals that the currently circulating strains look biologically different than the ones seen at the beginning of the pandemic. While many of the changes to the virus are perfectly benign, some strains seem to be more contagious, and some are better able to evade antibodies, a key part of the body’s defense system.
Intriguingly, the most bothersome changes all involve the virus’s spike protein, and they are sprouting up independently across continents, perhaps due to a phenomenon called convergent evolution.
The fear is that some of these so-called “variants of concern”—including newly reported ones in the United States—could diminish the power of our vaccine arsenal. That’s because people who have been vaccinated, or who gained immunity through natural infection, may still be vulnerable to these variants—a vulnerability that’s at odds with recommendations the U.S. Centers for Disease Control and Prevention released this week saying that the vaccinated people could safely gather indoors with other vaccinated people.
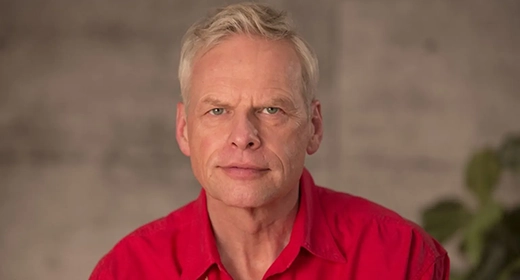
“The needle of public opinion is clearly tilted towards relaxation, but with the high rate of current infections in the U.S. and the variants of concern on the rise, we may regret it,” says Stuart C. Ray, an infectious disease professor at Johns Hopkins Medicine in Baltimore.
In response, vaccine makers are scrambling to study and manufacture variant-specific boosters. At the same time, the Biden administration has promised to make vaccinations available for every adult in the U.S. by the end of May.
The faster the coronavirus is brought under control, experts say, the fewer chances it has to mutate into more lethal and transmissible versions that could fuel another deadly wave.
U.S. homegrown variants
Over the past couple months, health officials have been focused on potentially dangerous variants that appeared in other countries. In December came news that a variant called B.1.1.7 was circulating in the United Kingdom. Then came reports of the B.1.351 variant that first appeared in South Africa and doesn’t respond as well to vaccines. There’s another disquieting variant called P.1 from Brazil that new research suggests could reinfect COVID-19 survivors.
All three of these variants have reached U.S. shores. According to the CDC’s latest count, there are 3,037 documented cases of the U.K. variant, 81 cases of the South African strain, and 15 of the Brazilian one in the country.
Now health officials are trying to gauge the threat of several domestic varieties, including ones originating in California and New York City. Infectious disease expert Anthony Fauci told host Margaret Brennan on Face the Nation that he was concerned about the recently documented spread of the variant B.1.526, which was first detected in Manhattan last month, because of the risk it might elude antibody protection from vaccines as well as other COVID-19 therapies.
The New York variant accounted for a quarter of the coronavirus genomes that were collected and sequenced in the New York region in February, according to research from a team at California Institute of Technology that has not yet been peer reviewed. In another preprint study, Columbia University researchers wrote: “this novel variant is surging, alarmingly, in our patient population over the past few weeks.”
In California, officials at Cedars-Sinai Medical Center in Los Angeles reported the presence of another potentially more contagious variant called CAL.20C that was first observed in July 2020 but not detected again in Southern California until October. Of the viral sequences that were collected statewide, this variant accounted for 35 percent of COVID-19 cases in January.
However, Adam Lauring, an infectious disease expert at the University of Michigan, cautions against getting too alarmed until more is known. Genetic surveillance is still ramping up in the U.S., and scientists are missing important data that can put the variants in context. In the U.K., researchers looked at hospital records and contact tracing in addition to genetic sequencing reports before suggesting in February that the B.1.1.7 variant causes a more severe form of the disease.
In the U.S., “the studies are small, and we have more to learn,” Lauring says. “It’s hard to know what’s concerning and what isn’t a big deal.”
The mystery of mutations
What is clear is that the viral variants are accumulating mutations faster than they did at the beginning of the pandemic and becoming more infectious, says Johns Hopkins Medicine’s Ray, who studies RNA virus evolution.
And what fascinates many scientists is that the lineages of the British, Brazilian, and South African variants all contain mutations that alter the biology of the spike protein, the part of the virus that invades a human cell and makes people sick. “They all changed three separate times on three separate continents within months of each other,” says Ray. Similar mutations were also found in the New York and California variants.
Although such changes might seem random, Paul Bieniasz, a virologist at Rockefeller University in New York City, suggests there are bigger forces at work. “It’s clear there’s convergent evolution going on,” says Bieniasz, referring to an evolutionary principle in which organisms independently evolve similar traits due to similar environments or pressures.
So many people have been infected that the virus has had trillions of opportunities to mutate, replicate, and evolve. The mutations that allow the virus to infect more people, or avoid antibodies, will be more successful and more difficult to snuff out. That’s why it makes sense all the variants of concern so far show changes to the spike protein, says Bieniasz.
In an eerily prescient study published in October, his team constructed a model showing that the coronavirus was able to mutate just enough in the spike protein to evade protective antibodies that are supposed to attach to it and block the virus from entering cells.
Bieniasz fears that such SARS-CoV-2 variants could make the virus less recognizable to the antibodies triggered by the current vaccines. Or these new strains could reinfect people who’d already recovered from a different strain of the coronavirus and extend the pandemic longer.
There is some good news, however. Despite the variants’ ability to evade some of our defenses, most of us have dozens of kinds of antibodies that can still provide protection. The mutations seen so far only cause a handful of them to lose their potency.
“What this means is that good vaccines will still work. Will they work as well? That is less clear,” says Bieniasz.
Better tracking
In the meantime, the U.S. government has pledged nearly $200 million to increase the nation’s virus sequencing capacity to track the emergence of new strains. In a white paper submitted to the White House, genetic sequencing companies and public and private labs urged the Biden administration to “rapidly deploy national genomic surveillance at scale” and set a goal of sequencing 5 percent of positive samples.
Making progress on this effort isn’t about technical capacity and acumen, says Christopher Mason, associate professor of computational genomics at Weill Cornell Medicine in New York City. “It’s about the logistics and the funding.”
Google, the Rockefeller Foundation, and seven academic institutions in the U.S. and Europe have also launched the Global.health database, which would collect details, including patients’ travel histories or onset of symptoms, to offer a more granular picture of how variants are spreading
Yet generating more sequencing data provides only one clue into how the coronavirus is behaving. “We need more sequencing, but it has to be smartly targeted to identify the virus and what’s driving the virus to mutate and change,” adds Rick Bright, senior vice president of pandemic prevention and response at the Rockefeller Foundation. “We need geographic representation—not just in New York City, but also rural areas.”
This would provide a snapshot of a virus emerging among vaccinated people or within certain vulnerable communities; for instance, one study found that the CAL.20C variant made up more than half of January cases in the predominantly Latino community in San Francisco’s Mission District—up from just 16 percent in November. That’s valuable information for public health officials to target and contain the spread.
“We’d be able to stay two steps ahead of the virus instead of five steps behind it,” adds Bright, former director of the Biomedical Advanced Research and Development Authority.
Such an enhanced system could even provide an early warning system for future disease outbreaks and other biological attacks, says Andrew Weber, senior fellow at the Council on Strategic Risks and former assistant secretary for nuclear, chemical, and biological defense program at the U.S. Defense Department.
“If you have an ongoing surveillance program, you’ll detect the anthrax and Ebola threats,” he says. “It’s about reducing the time to discovery and having rapid medical countermeasures to respond effectively.”
For now, though, the greatest priority is to slow the rate of mutation by getting people vaccinated and controlling the spread of COVID-19, says Ray. Otherwise, we risk the virus having a chance to evolve greater resistance strategies. “Then,” he says, “we’ll have a bigger problem on our hands.”