An Overview of Research Conducted by the HeartMath Institute
Heart-Brain Communication
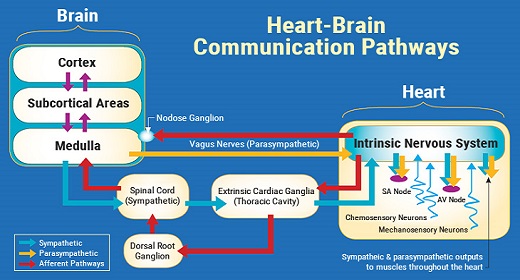
Traditionally, the study of communication pathways between the head and heart has been approached from a rather one-sided perspective, with scientists focusing primarily on the heart’s responses to the brain’s commands. We have learned, however, that communication between the heart and brain actually is a dynamic, ongoing, two-way dialogue, with each organ continuously influencing the other’s function. Research has shown that the heart communicates to the brain in four major ways: neurologically (through the transmission of nerve impulses), biochemically (via hormones and neurotransmitters), biophysically (through pressure waves) and energetically (through electromagnetic field interactions). Communication along all these conduits significantly affects the brain’s activity. Moreover, our research shows that messages the heart sends to the brain also can affect performance.
The heart communicates with the brain and body in four ways:
- Neurological communication (nervous system)
- Biochemical communication (hormones)
- Biophysical communication (pulse wave)
- Energetic communication (electromagnetic fields)
Some of the first researchers in the field of psychophysiology to examine the interactions between the heart and brain were John and Beatrice Lacey. During 20 years of research throughout the 1960s and ’70s, they observed that the heart communicates with the brain in ways that significantly affect how we perceive and react to the world.
In physiologist and researcher Walter Bradford Cannon’s view, when we are aroused, the mobilizing part of the nervous system (sympathetic) energizes us for fight or flight, which is indicated by an increase in heart rate, and in more quiescent moments, the calming part of the nervous system (parasympathetic) calms us down and slows the heart rate. Cannon believed the autonomic nervous system and all of the related physiological responses moved in concert with the brain’s response to any given stimulus or challenge. Presumably, all of our inner systems are activated together when we are aroused and calm down together when we are at rest and the brain is in control of the entire process. Cannon also introduced the concept of homeostasis. Since then, the study of physiology has been based on the principle that all cells, tissues and organs strive to maintain a static or constant steady-state condition. However, with the introduction of signal-processing technologies that can acquire continuous data over time from physiological processes such as heart rate (HR), blood pressure (BP) and nerve activity, it has become abundantly apparent that biological processes vary in complex and nonlinear ways, even during so-called steady-state conditions. These observations have led to the understanding that healthy, optimal function is a result of continuous, dynamic, bidirectional interactions among multiple neural, hormonal and mechanical control systems at both local and central levels. In concert, these dynamic and interconnected physiological and psychological regulatory systems are never truly at rest and are certainly never static.
For example, we now know that the normal resting rhythm of the heart is highly variable rather than monotonously regular, which was the widespread notion for many years. This will be discussed further in the section on heart rate variability (HRV).
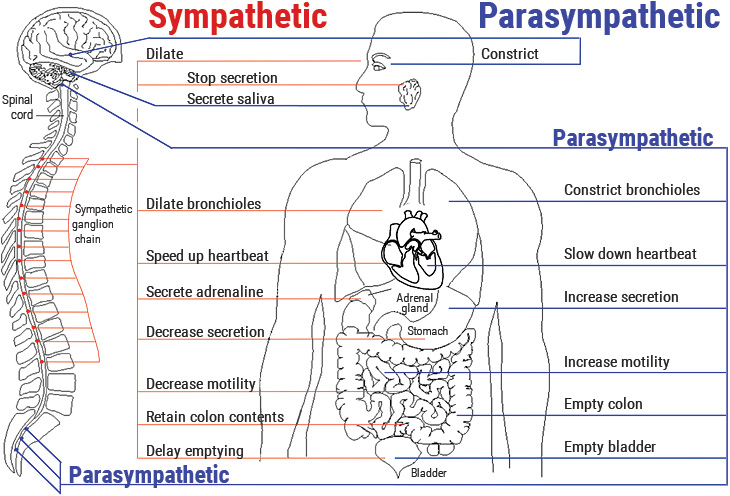
The Laceys noticed that the model proposed by Cannon only partially matched actual physiological behavior. As their research evolved, they found that the heart in particular seemed to have its own logic that frequently diverged from the direction of autonomic nervous system activity. The heart was behaving as though it had a mind of its own. Furthermore, the heart appeared to be sending meaningful messages to the brain that the brain not only understood, but also obeyed. Even more intriguing was that it looked as though these messages could affect a person’s perceptions, behavior and performance. The Laceys identified a neural pathway and mechanism whereby input from the heart to the brain could inhibit or facilitate the brain’s electrical activity. Then in 1974, French researchers stimulated the vagus nerve (which carries many of the signals from the heart to the brain) in cats and found that the brain’s electrical response was reduced to about half its normal rate.[1] This suggested that the heart and nervous system were not simply following the brain’s directions, as Cannon had thought. Rather, the autonomic nervous system and the communication between the heart and brain were much more complex, and the heart seemed to have its own type of logic and acted independently of the signals sent from the brain.
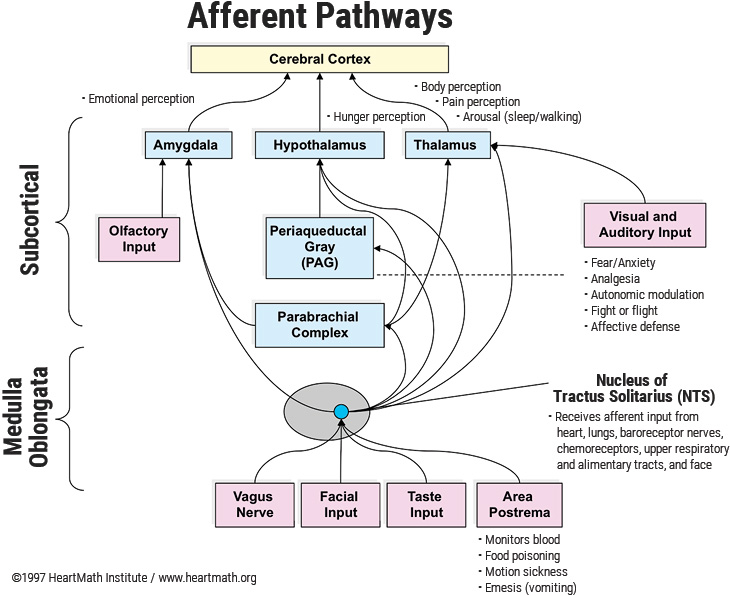
While the Laceys research focused on activity occurring within a single cardiac cycle, they also were able to confirm that cardiovascular activity influences perception and cognitive performance, but there were still some inconsistencies in the results. These inconsistencies were resolved in Germany by Velden and Wölk, who later demonstrated that cognitive performance fluctuated at a rhythm around 10 hertz throughout the cardiac cycle. They showed that the modulation of cortical function resulted from ascending cardiovascular inputs on neurons in the thalamus, which globally synchronizes cortical activity.[2, 3] An important aspect of their work was the finding that it is the pattern and stability of the heart’s rhythm of the afferent (ascending) inputs, rather than the number of neural bursts within the cardiac cycle, that are important in modulating thalamic activity, which in turn has global effects on brain function. There has since been a growing body of research indicating that afferent information processed by the intrinsic cardiac nervous system (heart-brain) can influence activity in the frontocortical areas[4-6] and motor cortex,[7] affecting psychological factors such as attention level, motivation,[8] perceptual sensitivity[9] and emotional processing.[10]
Neurocardiology: The Brain On the Heart
While the Laceys were conducting their research in psychophysiology, a small group of cardiologists joined forces with a group of neurophysiologists and neuroanatomists to explore areas of mutual interest. This represented the beginning of the new discipline now called neurocardiology. One of their early findings is that the heart has a complex neural network that is sufficiently extensive to be characterized as a brain on the heart (Figure 1.2).[11, 12]The heart-brain, as it is commonly called, or intrinsic cardiac nervous system, is an intricate network of complex ganglia, neurotransmitters, proteins and support cells, the same as those of the brain in the head. The heart-brain’s neural circuitry enables it to act independently of the cranial brain to learn, remember, make decisions and even feel and sense. Descending activity from the brain in the head via the sympathetic and parasympathetic branches of the ANS is integrated into the heart’s intrinsic nervous system along with signals arising from sensory neurons in the heart that detect pressure, heart rate, heart rhythm and hormones.
The anatomy and functions of the intrinsic cardiac nervous system and its connections with the brain have been explored extensively by neurocardiologists.[13, 14] In terms of heart-brain communication, it is generally well-known that the efferent (descending) pathways in the autonomic nervous system are involved in the regulation of the heart. However, it is less appreciated that the majority of fibers in the vagus nerves are afferent (ascending) in nature. Furthermore, more of these ascending neural pathways are related to the heart (and cardiovascular system) than to any other organ.[15] This means the heart sends more information to the brain than the brain sends to the heart. More recent research shows that the neural interactions between the heart and brain are more complex than previously thought. In addition, the intrinsic cardiac nervous system has both short-term and long-term memory functions and can operate independently of central neuronal command.
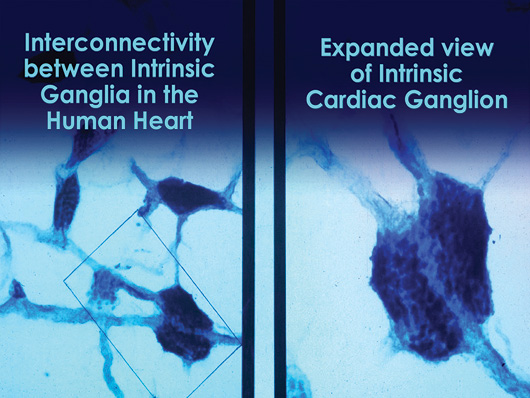
Courtesy of Dr. J. Andrew Armour
Once information has been processed by the heart’s intrinsic nervous system, the appropriate signals are sent to the heart’s sinoatrial node and to other tissues in the heart. Thus, under normal physiological conditions, the heart’s intrinsic nervous system plays an important role in much of the routine control of cardiac function, independent of the central nervous system. The heart’s intrinsic nervous system is vital for the maintenance of cardiovascular stability and efficiency and without it, the heart cannot function properly. The neural output, or messages from the intrinsic cardiac nervous system travels to the brain via ascending pathways in the both the spinal column and vagus nerves, where it travels to the medulla, hypothalamus, thalamus and amygdala and then to the cerebral cortex.[5, 16, 17] The nervous-system pathways between the heart and brain are shown in Figure 1.3 and the primary afferent pathways in the brain are shown in Figure 1.4.
Had the existence of the intrinsic cardiac nervous system and the complexity of the neural communication between the heart and brain been known while the Laceys were conducting their paradigm-shifting research, their theories and data likely would have been accepted far sooner. Their insight, rigorous experimentation and courage to follow where the data led them, even though it did not fit the well-entrenched beliefs of the scientific community of their day, were pivotal in the understanding of the heart-brain connection. Their research played an important role in elucidating the basic physiological and psychological processes that connect the heart and brain and the mind and body. In 1977, Dr. Francis Waldropin, director of the National Institute of Mental Health, stated in a review article of the Laceys’ work, “Their intricate and careful procedures, combined with their daring theories, have produced work that has stirred controversy as well as promise. In the long run, their research may tell us much about what makes each of us a whole person and may suggest techniques that can restore a distressed person to health.”
The Heart as a Hormonal Gland
In addition to its extensive neurological interactions, the heart also communicates with the brain and body biochemically by way of the hormones it produces. Although not typically thought of as an endocrine gland, the heart actually manufactures and secretes a number of hormones and neurotransmitters that have a wide-ranging impact on the body as a whole.
The heart was reclassified as part of the hormonal system in 1983, when a new hormone produced and secreted by the atria of the heart was discovered. This hormone has been called by several different names – atrial natriuretic factor (ANF), atrial natriuretic peptide (ANP) and atrial peptide. Nicknamed the balance hormone, it plays an important role in fluid and electrolyte balance and helps regulate the blood vessels, kidneys, adrenal glands and many regulatory centers in the brain.[18] Increased atrial peptide inhibits the release of stress hormones,[19] reduces sympathetic outflow[20]and appears to interact with the immune system.[21] Even more intriguing, experiments suggest atrial peptide can influence motivation and behavior.[22]
It was later discovered the heart contains cells that synthesize and release catecholamines (norepinephrine, epinephrine and dopamine), which are neurotransmitters once thought to be produced only by neurons in the brain and ganglia.[23] More recently, it was discovered the heart also manufactures and secretes oxytocin, which can act as a neurotransmitter and commonly is referred to as the love or socialbonding hormone. Beyond its well-known functions in childbirth and lactation, oxytocin also has been shown to be involved in cognition, tolerance, trust and friendship and the establishment of enduring pair-bonds. Remarkably, concentrations of oxytocin produced in the heart are in the same range as those produced in the brain.