A brief review of the growing body of knowledge of vitamin D…
OMNS (Feb. 17, 2022) The Harvard led Vitamin D and Omega 3 trial (VITAL), recently published findings showing a meaningful (22%) and statistically significant (p = 0.05, Hazard ratio = 0.78 95% CI = 0.61 – 0.99) reduction in the incidence of autoimmune disease in older adults taking 2000 IU (50 mcg) per day for 5 years. [1] This was a large nationwide study involving 12,786 men 50 years or older and 13,085 women 55 years or older. It was a randomized double blind, placebo-controlled trial. The British Medical Journal notes, “The clinical importance of this trial is high because these are well tolerated, non-toxic supplements, and other effective treatments to reduce the incidence of autoimmune diseases are lacking”. In 2017, the National Institutes of Health (NIH) estimated that 23.5 million Americans, >7% of the population, suffered from an autoimmune disease. The NIH noted that the prevalence appeared to be rising. [2]
Illustrating the high prevalence of vitamin D deficiency and insufficiency in the USA, 13% of participants in the VITAL trial had vitamin D levels < 20 ng/mL (50 nmol/L) at the start of the trial, and 45% had levels < 30 ng/mL (75 nmol/L). A subgroup of participants (1,644 people) had vitamin D levels tested one year into the study. In aggregate, participants taking 2000 IU vitamin D had an increase of 40% in vitamin D levels to 41.8 ng/mL (104.5 nmol/L), while participants in the soybean oil placebo group remained similar to baseline (30.7 ng/mL, 77.1 nmol/L). Strengths of this study include its size and diversity; its design as a prospective, placebo controlled, randomized trial — the “gold standard” for medical drug studies; its baseline measurement of blood levels of vitamin D and follow-up testing of a sample of participants, rather than relying on intake estimates; the use of a meaningful, safe dose more than double the US RDA for vitamin D, and its duration with a median follow-up time of 5.3 years.
“P values” are an expression of the degree of probability that the results of an experiment testing a hypothesis are due to chance. Generally speaking, the lower the P value, the higher the reliability of the data.
But nutrient studies require different approaches than drug studies. [3,4,5] A weakness of the VITAL trial was the absence of evaluation of synergistic nutrients. Additionally, with appreciation for Roger Williams’ principle of biochemical individuality, [6] it would have been interesting and helpful to compare the outcomes for each range of vitamin D levels achieved after the fixed dose intervention (e.g. stratifying participants by vitamin D levels achieved < 20, 20 – 29, 30-39, 40-49, 50-59). However, this would have required more measurements, thus increasing the expense of the trial.
The 3 Ds for vitamin D (and any nutrient) assessments:
Dose – how much of the nutrient reached the blood/tissue; whether the individual achieved and maintained sufficient or therapeutic levels.
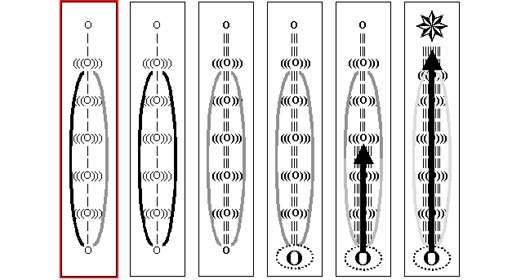
|
US RDA (2010) |
Recommendation of 220 vitamin D experts [7] |
Personal D3 supplementation of 193 vitamin D experts [7] |
|
|
0 – 12 months |
400 IU / day |
2000 – 4000 IU/day |
Range = 0 – 50,000 IU/day |
|
1 – 70 years |
600 IU / day |
||
|
71+ years |
800 IU / day |
||
|
Pregnant or |
600 IU / day |
||
| People with kidney disease should monitor vitamin D levels closely | |||
| Adjusting sunlight exposure, D3 intake, and co-factors to maintain vitamin D levels in the 40-60 ng/mL range is associated with lower risk of autoimmunity, respiratory disease, and other illnesses. Blood levels up to 100 ng/mL are generally safe with adequate vitamin K2. | |||
| Daily intake necessary from all sources (sunlight, food, and/or supplementation) of vitamin D for 97.5% of people to reach: 20 ng/mL = 3,875 IU D3 (97 mcg); 30 ng/mL = 6200 D3 (155 mcg) [7] | |||
Duration – how long sufficient or therapeutic levels were maintained. Vitamin D has extensive epigenetic effects, impacting over 3,000 genes. It has been estimated that as much as 3-4% of the genome may be influenced by vitamin D. These genetic influences may be especially important during fetal development. [8] The half-life of the active form of vitamin D is about 4 hours, and the half-life of the pre-hormone form of vitamin D is 2-3 weeks. However, it may take even longer for the effects of proteins from genes upregulated and downregulated by vitamin D to make their biological impact. Bruce Ames’ concept of “longevity proteins” applies. [9] With saturation of a full set of nutrients, cell metabolism is able to expand from production of only survival proteins to producing additional proteins he called “longevity proteins”. For these reasons, it is important to maintain vitamin D in the healthy range on an ongoing basis rather than waiting until illness occurs. When rescue therapy is needed, calcifediol (25OHD) increases active vitamin D levels more rapidly than cholecalciferol (D3). [10-12] (see https://www.orthomolecular.org/resources/omns/v17n17.shtml and https://www.orthomolecular.org/resources/omns/v16n55.shtml for discussions of nutritional support in critical illness).
Dynamic interactions – were sufficient levels of synergistic cofactors maintained? Magnesium is necessary in eight steps of vitamin D metabolism. [13,14] Intracellular selenocysteine can also be a rate limiting factor in vitamin D production and function. Increasing glutathione and cysteine can increase production of vitamin D even without vitamin D intake or sunlight exposure. In turn, vitamin D increases production of several selenoproteins. [15-17] Vitamin C and zinc also assist actions of vitamin D, and it is important to balance vitamin D with vitamin K2 to ensure mobilized calcium gets where it is needed rather than being deposited in arteries. 100 mcg K2 for every 5000 IU D3 is a good ratio for wellness. [18,19]
In research, controls matter too. This same VITAL study also looked at the effects of supplementing 1000 mg/day of omega-3 vs. placebo. A 15% reduction in the incidence of autoimmune disease was seen compared to the control group. However, this did not reach statistical significance. Interestingly, olive oil, which is known to be anti-inflammatory and a source of vitamin K, was used as the placebo for comparison. It is possible that the choice of a non-inert placebo blunted the signal of true benefit from the omega-3 intervention.
Vitamin D: influence on the immune system
The VITAL study adds important support on the benefits of vitamin D for the immune system. Vitamin D regulates calcium and phosphate homeostasis in the body. Calcium is important for much more than strong bones. [20-23] Mobilized ionized calcium is essential for muscle contractions, nerve impulses, cell signalling, blood clotting, immune function, and catalyzing hundreds of enzymatic reactions throughout the body. Nearly all cells in the body have vitamin D receptors (VDRs). Intestine, bone, kidney, parathyroid glands, and immune cells (T cells, B cells, Dendritic Cells, Macrophages) have high levels of VDRs. The CYP27B1 enzyme which produces the active form of vitamin D and the ligand for VDR is also widely expressed in many cells throughout the body. The liver and kidney produce much of the active vitamin D in the body, however activated immune cells will also produce 1,25(OD)2D when the 25OHD substrate is present for conversion into the active hormone. Parathyroid Hormone (PTH) regulates the production of the active form of vitamin D in non-immune cells. Active vitamin D production in immune cells is not influenced by PTH, but is instead regulated by cytokines and the availability of the prehormone 25OHD in the local cellular environment.
Vitamin D has important influences on many phases in the innate branch of the immune system (cellular, complement, antimicrobial peptides, lectins, non-antibody producing aspects of immunity), and also in the adaptive branch of the immune system (antibody-producing aspects of immunity). The adaptive branch of the immune system has two major phases. The effector phase involves antibody production while the regulatory phase involves removal of B cells producing antibodies that cross-react with self-cells. The antibody-antigen lock and key fit isn’t always exact. Even healthy people have self-reactive B cell clones. [24] Similarity between a “foreign” antigen and a host cell membrane element may exist or an antibody may overlap the membrane portion of a neoantigen-membrane complex. When B cells with these self-reacting or self-cross-reacting antibodies are stimulated to mass divide and produce their antibodies, they must be destroyed by the regulatory immune cells (Tregs) to minimize self-injury. Imbalance or dysfunction in the regulatory phase of the adaptive immune response is the major mechanism of autoimmune diseases in humans. [25] Interestingly, several sensitive areas of the body, the brain, anterior chamber of the eyes, and testes, are devoid of adaptive immune responses. The risk of collateral damage from antibody production in these areas is too great.
The active form of vitamin D: [26,27]
- Increases production of cathelicidin and defensins
- Decreases the maturation of dendritic cells, the expression of HLA DR antigen presenting molecules, and expression of co-stimulation molecules such as CD40, CD80, and CD86
- Decreases Th1, Th9, Th17 lymphocytes, decreasing IL-2, IL-6, IFN-gamma, IL-12, IL-17, IL-23
- Increases Treg production and production of the cytokine IL-10
- Increases production and maintenance of immune memory cells
The overall effect is a stronger innate immune response, and a safer adaptive immune response.
A short history of clinical observations about vitamin D
- In 1903, Niels Ryberg Finsen received the Nobel Prize in Physiology and Medicine “in recognition of his contribution to the treatment of diseases…with concentrated light radiation, whereby he has opened a new avenue for medical science.” [28]
- Sanatoriums and cod liver oil were common treatments for tuberculosis and other infections for many decades. [29]
- Two studies in South Carolina in the past decade showed significant reductions in preterm births (57% fewer 95% CI RR = 0.22 – 0.83, and 62% fewer p = 0.002) in women with vitamin D levels ≥ 40 ng/mL compared to women with vitamin D levels < 20 ng/mL. [30,31]
- A pooled analysis of over 2300 women ≥ 55 years of age from a randomized controlled trial and a prospective cohort study showed participants with a vitamin D level ≥ 40 ng/mL had a 67% lower risk of invasive cancer compared to participants with a vitamin D level < 20 ng/mL. [32] Similar results were seen with breast cancer when people with vitamin D levels >60 ng/mL were compared to people with vitamin D levels < 20 ng/mL. [33]
- In 2018, the VITAL trial research group published a conclusion that 2000 IU of supplemental vitamin D per day had no impact on cancer risk. [34] However, their data show a 25% reduction in cancer risk after the first 2 years of the study. [35]
- A meta-analysis of 32 studies was published in 2014 showing a greater risk of all-cause mortality in people with a vitamin D level = 30 ng/mL compared to those with a vitamin D level > 30 ng/mL (Hazard Ratio = 1.9, 95% CI = 1.6 – 2.2, p=0.001). [36]
- From Tuberculosis to COVID
- Two recent Spanish studies on treatment of acute Covid-19 showed the efficacy of calcifediol for reducing ICU admission and mortality. [11-12]
- In February 2022, a retrospective study in Israel of 253 consecutive adults admitted to the hospital for treatment of SARS-CoV-2 infection with a vitamin D measurement available 14 – 730 days prior to admission showed a greater risk of severe illness (48.1% vs. 10%) and death (25.6% vs. 5%) in those with vitamin D levels < 20 ng / mL vs. ≥ 20 ng / mL. [33] This was a follow up study to a large retrospective case-controlled population study associating vitamin D deficiency with a higher risk of Covid-19 infection. [37,38] Studies in three different countries showed an association between selenium deficiency and severe SARS-CoV-2 disease [39-41]. Even though relationships between vitamin D and selenoproteins are now established, no studies measuring both selenium and vitamin D in SARS-CoV-2 patients have been published.
- A study published in February 2022 from Mexico showed improved survival of high risk SARS-CoV-2 patients admitted to the hospital when given extra nutritional support. [42] 7 (17.5%) of 40 patients given standard of care died, while 1 (2.5%) of 40 patients given special nutritional support died. The extra nutritional support consisted of:
- B-complex: 10 mg of cyanocobalamin, 100 mg of thiamin, and 100 mg of pyridoxine administered intramuscularly every 24 h for the first 5 days.
- One envelope package taken orally after morning meals and another after evening meals, diluted in 400 mL of water each, during the whole intervention for a maximum of 21 days. Each envelope contained: Spirulina Maxima 2.5 g, folic acid 5 mg, glutamine 5 g, vegetable protein 10 g, brewer’s yeast, amaranth, ascorbic acid 1 g, zinc 20 mg, selenium 100 mcg, cholecalciferol (D3) 2000 IU, resveratrol 200 mg, Omega-3 fatty acids 1 g, L-Arginine 750 mg, inulin 20 g, and magnesium 400 mg.
- Probiotics: Saccharomyces boulardii 500 mg daily for 6 days orally
- A robust series of publications from 2021 showed the benefits of vitamin D for Covid-19 and other major diseases. See “Top Vitamin D Papers in 2021: Benefits ignored at a time they are most needed” by William B. Grant, PhD https://orthomolecular.org/resources/omns/v18n02.shtml
Summary
Vitamin D is important for a wide range of functions in human biology from conception onward. We now have more evidence pointing towards the importance of maintaining a vitamin D level in the 40-60 ng/mL range, along with maintaining adequate levels of synergistic nutrients to fight infections, sustain helpful immunity, and also to prevent harmful autoimmune reactions.