by Ocean Robbins: When we think about the causes of arthritis, we typically picture an older person whose cartilage has been worn down by time, use, or injury…
We are proud to announce a new partnership with John and Ocean Robbins and the Food Revolution to bring our readers Summits, Seminars and Masterclasses on health, nutrition and Earth-Conscious living.
Sign Up Today For the Healthy Brain Masterclass
But one particular form — rheumatoid arthritis — is caused by the body’s immune system attacking its own connective tissue between joints.
Rheumatoid arthritis (RA) is a chronic, systemic autoimmune disease that results in joint inflammation and subsequent cartilage degradation. An estimated one percent of the world’s population and as many as 1.3 million Americans, according to the Rheumatoid Arthritis Support Network, have RA. Patients with RA can suffer from fatigue, pain, stiffness, and impaired physical function, all of which can lead to severe disability.
However, unlike other types of arthritis, such as osteoarthritis, RA is not primarily caused by wear and tear. There are other factors at play besides age in the development of this type of arthritis, which often begins between ages 30 and 60.
With RA, the body attacks the connective tissue between joints that normally would help them move. This causes pain, swelling, and stiffness which limits movement and damages bones over time.
While RA is predominantly associated with joint tissue inflammation, as an autoimmune connective tissue disorder, RA can attack other types of connective tissue leading to complications with the lungs, heart, skin, and eyes, too.
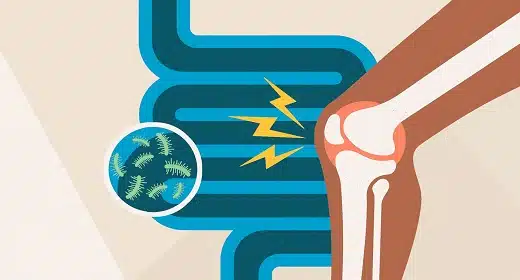
However, like other types of autoimmune disorders and chronic diseases, more and more research is telling us that changes to your diet and the state of your gut might play an important role in your chances of developing RA, and effectively managing or reversing it if you do.
In this article, we’ll look at typical RA treatments and alternatives — and the link between rheumatoid arthritis, the gut, and what’s at the end of our forks.
What Causes Rheumatoid Arthritis?
There’s no definitive answer as to what causes autoimmune diseases like RA. However, a growing body of evidence is pointing to a few key factors.
While each situation is highly individualized, many scientists suspect the following three major factors may play a role in causing rheumatoid arthritis:
- Genetics: According to Cleveland Clinic, RA is “more common among people designated female at birth” or who have a direct family member who is affected by the disease.
- Infections: Certain microbes, like Epstein-Barr virus (infectious mononucleosis) and Proteus mirabilis (which causes some UTIs) are linked to a greater risk of RA and more problematic symptoms.
- Balance of the intestinal microbiome: Evidence from the Journal of Immunology Research shows that your gut may be the most decisive factor in RA development. An imbalance of intestinal bacteria due to lifestyle and environmental factors can be a huge driver of rheumatoid arthritis. And since you have little control over your genetics (unless, of course, you invent a time machine and try to change who your parents were — which might create a new set of problems), or over what infections you might be exposed to, this is the area we’re going to focus on the most.
The Connection Between Gut Health and Rheumatoid Arthritis
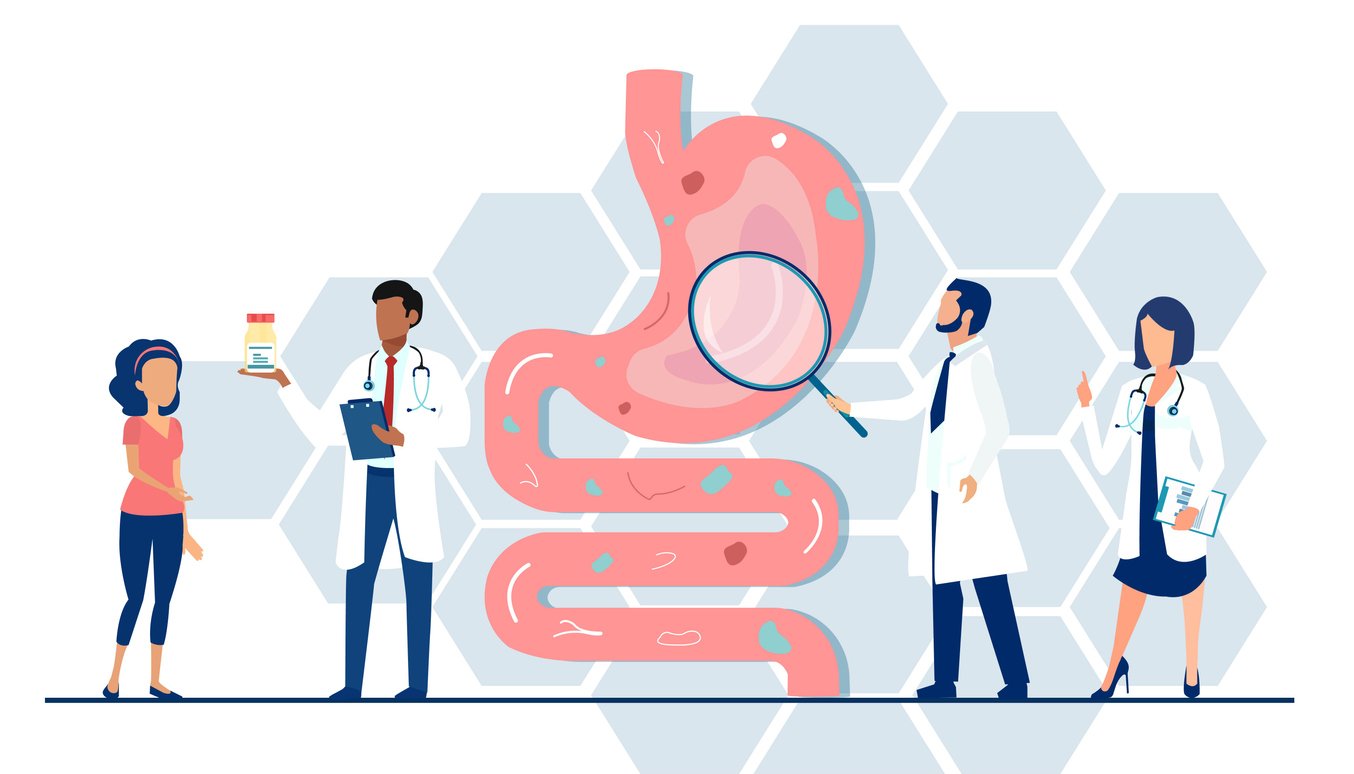
There’s a growing and exciting body of research that confirms a strong link between the health of your gut and the condition of your joints — and overall health. But this isn’t exactly a new idea. Hippocrates, the ancient Greek healer known as the father of medicine, theorized that all diseases originate in the gut. (To be fair, he also taught that the uterus wandered around the body looking for warmth, so he didn’t always bat a thousand with his conjectures.)
The digestive microbiome is responsible for helping to break down food and produce vitamins, nutrients, and hormones that you need to stay healthy. Even more incredibly, 70% of your immune system is in your gut, where it trains immune cells, fends off harmful pathogens, and regulates immune function throughout your body.
Autoimmune diseases like RA are characterized by an overreaction of the immune system. (If another metaphor would help, it’s like a smoke detector that triggers the sprinkler system every time you boil water or make toast.)
Because gut microbiota helps regulate immune system stability and function, it makes sense that immune dysfunction could stem from an impaired microbiome. In fact, a 2021 study at the Mayo Clinic’s Center for Individualized Medicine found that the health of a RA patient’s gut microbiome could predict the improvement of their arthritis over time.
Another study found an interesting link between a bacteria known as P. copri and rheumatoid arthritis. In 75% of individuals suffering from RA, this microbe was in abundance in their fecal samples. Researchers hypothesize that having too much of this bacterial strain in the gut could be one of the potential causes of RA. The research is increasingly compelling that there is a strong connection between gut microbes and disease outcomes for rheumatoid arthritis and other autoimmune conditions.
How Is Rheumatoid Arthritis Commonly Treated?
RA symptoms can be debilitating and lead to lower quality of life, especially during a flare-up when symptoms are at their worst. Over time, the disease can become systemic and eventually attack vital organs, causing disease complications and death.
Because of this, treatments for RA are usually aggressive. And although there is no known cure, the first line of defense often includes medications prescribed to reduce joint inflammation, relieve pain, and prevent or slow joint and tissue damage.
Common RA treatments include:
- NSAIDs
- Steroids
- Disease-modifying antirheumatic drugs (DMARDs)
- Biologic agents
However, many drugs used to treat rheumatoid arthritis have potentially serious side effects, like liver and kidney damage, increased blood pressure, and even the development of type 2 diabetes, among others.
If medications fail to stop the progression of tissue damage or have to be stopped due to side effects, surgery is typically the second line of treatment and can include:
- Total joint replacement
- Tendon repair
- Joint fusion
Does just reading those descriptions make you think, “These procedures don’t sound fun at all”? If so, you’re not alone. Because the treatment options for RA are potentially dangerous and carry serious side effects, many patients turn to complementary medicine, looking for additional sources of relief and treatment options that bring fewer side effects.
Can Dietary Changes Help with Rheumatoid Arthritis?

While genetic and infection-based causes of RA are mostly out of your control, you do get to decide what you eat.
And that’s good news because it turns out that nutritional therapy can be a powerful tool for managing RA. According to a 2017 study in Frontiers in Nutrition, dietary changes can reduce RA flare-ups. In the same study, scientists found that nutritional interventions can also delay RA progression. The researchers drew a direct connection between gut health, diet, and the symptoms and development of RA.
Is it metaphor time again? OK — it’s like your microbiome is full of trillions of employees, many of whom train, manage, and recruit the workers who run the immune system. And they eat all their meals at the company cafeteria. If you serve them abundant and nutritious fare, they do their jobs well. If you give them junk food, quality goes out the window, and pretty much anything goes.
Plant-Based Diets and Rheumatoid Arthritis
So, what types of dietary changes help with rheumatoid arthritis the most?
Specifically, people suffering from rheumatoid arthritis are encouraged to focus on eating plenty of colorful, whole foods, especially as part of a plant-based diet. Both vegetarian and vegan diets may help reduce inflammation and pain in RA. For example, a 2015 study found a 3-week vegan lifestyle intervention resulted in a 33% reduction in the level of C-reactive protein, a key marker of inflammation. Similarly, a randomized clinical trial found that a gluten-free, vegan diet decreases immunoglobulin G (IgG) for gliadin and whey — which are key proinflammatory antibodies.
Fruits and Vegetables for Rheumatoid Arthritis

Reducing inflammation and addressing symptoms of the existing disease is one thing, but what if diet might actually be able to prevent some RA cases? Excitingly, many fruits and vegetables may be protective against the development of RA. Specifically, a higher intake of certain carotenoids from fresh produce, as well as foods containing beta-cryptoxanthin from citrus and zeaxanthin from leafy greens, have been linked to lower rates of RA. One study involving more than 25,000 people found that the people who ate the most carotenoids had half the risk of developing inflammatory polyarthritis, compared with the people who ate the least.
Foods that are high in carotenoids include bell peppers, broccoli, cantaloupe, avocado, corn, kale, spinach, summer squash, and pumpkin.
Animal Protein and Rheumatoid Arthritis
Several studies have found improvements in RA symptoms like joint pain, stiffness, swelling, and limitation in function with diets low in arachidonic acid, an omega-6 fatty acid primarily found in animal products. Furthermore, a reduction in animal protein is linked to lower inflammatory markers and increased insulin sensitivity. By replacing animal products with low-inflammatory, nutrient-rich plant foods, you may be fueling your body with what it needs to heal.
A whole foods, plant-based diet is, of course, naturally low in (or free of) animal products. This eating path is also low in saturated fat and rich in inflammation-busting compounds. It’s also higher in fiber, which turns out to be critical to the health of your microbiome.
Prioritize High-Fiber, Whole Foods

Fruits and veggies are healthy for a thousand reasons, including that they’re just the kind of foods that your “good” gut bugs need to thrive. Research tells us that the bacteria and yeasts most beneficial to humans actually get stronger when fed colorful plant-based foods that are rich in fiber.
In RA patients, studies have shown that fiber improves gut bacteria composition and increases bacterial diversity. The resulting boost in gut health reduces levels of inflammation and joint pain.
Sadly, less than 5% of people get enough fiber in their daily diets. And adjusting to a high-fiber diet can take some work, so to help you figure out how to get more fiber, we’ve put together some resources in our article on why fiber is good for you.
When it comes to the inflammation that underlies RA, new research is beginning to look at the connection between intestinal and joint inflammation as well as the influence of high-fiber, low-glycemic index foods on inflammatory gene expression. Below are some recipes for rheumatoid arthritis to help you get started.
Recipes to Help Calm or Prevent Rheumatoid Arthritis
These delicious plant-based recipes contain healthy and anti-inflammatory omega-3 fats and nourishing antioxidants and micronutrients. Plus, they use highly supportive plant foods like cruciferous veggies and nourishing anti-inflammatory herbs like turmeric to support a healthy gut, so you can get back to enjoying life to the fullest!
1. Ocean’s Savory Oatmeal

Ocean’s Savory (Instant Pot) Oatmeal has all the plant-based goodness to help fight inflammation, improve gut health, and keep you mobile. Is savory oatmeal new to you? You’re in for a treat! It’s filled with fiber from the oats, seeds, and kale; protein from the pumpkin and hemp seeds; and phytonutrients from the kale, alliums (garlic and onion), spices, and seeds. To top it off, ground turmeric adds a touch of earthy flavor and boatloads of phytonutrients to make this an anti-inflammatory breakfast of champions. Plus, this recipe is nourishing, tasty, and a fun way to use that Instant Pot!
2. Purple Powered Lunch Bowl with Crispy Chickpeas

Support your joint health with this highly nutritious (and colorful!) anti-inflammatory Purple Powered Lunch Bowl with Crispy Chickpeas. This bowl is full of purple foods (as well as a few other colors!) indicating its phytonutrient power. Many of these phytonutrients act as antioxidants, scavenging free radicals and reducing inflammation to help support mobile joints and an active lifestyle. Some of the most beneficial types of veggies for joint health are cruciferous vegetables, and this bowl has a few! Kale and red cabbage contain a compound called sulforaphane which, when eaten regularly, has anti-arthritic capabilities that help to block joint inflammation and slow cartilage deterioration. Not only is this bowl packed with plant-nourishing goodness, but it’s also full of flavor, texture, and other essential nutrients that contribute to overall health.
3. Cherry Chia Cacao Pudding Parfait

This Cherry Chia Cacao Pudding Parfait is creamy, nourishing, and filled with healthy omega-3 fats that can help reduce swelling, tenderness, and morning stiffness of joints among people with rheumatoid arthritis. The cherries included in this nutritious treat are packed with antioxidants that also help to reduce pain and inflammation in joints (you might call this part of the recipe the beneficial “cherry on top!”). This powerhouse combo is not only beneficial for your body, but it’s tasty, too! Enjoy it for breakfast, dessert, or as a scrumptious afternoon pick-me-up.
Diet Can Help with RA
Rheumatoid arthritis can be debilitating, especially when pain and inflammation make it difficult to hold down a job or care for family members. Treatments are often aggressive and can have their own set of side effects, so many people look to lifestyle factors and complementary therapies for relief. Diet can be one of the most important interventions in preventing and managing rheumatoid arthritis because inflammation and gut dysbiosis seem to play a part in its development and progression. A whole foods, plant-based diet, in particular, is a low-risk option with potentially significant benefits for RA. Eating this way can reduce inflammatory markers, decrease the risk of flare-ups, and improve the quality of life for those suffering from rheumatoid arthritis — and for just about everyone else, too.