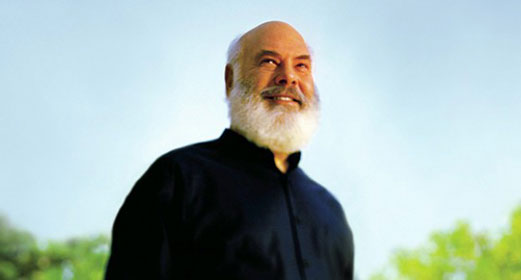
by Dr. Andrew Weil: On its surface, the cause of the Western world’s obesity epidemic seems simple: People are eating too many calories and getting too little calorie-burning exercise; the imbalance manifests as excess fat. But this explanation is too simple. Even low-calorie diets and vigorous exercise fail to work in the long term for at least some people.
But this explanation is too simple. Even low-calorie diets and vigorous exercise fail to work in the long term for at least some people.
Here’s why: Exercise, while vital to good health, is a poor exclusive means of weight control. Excess exercise tends to be counterbalanced by excess hunger, exemplified by the phrase “working up an appetite.” A few people with extraordinary willpower can resist such hunger day after day, but for the vast majority, weight loss through exercise is a flawed option.
Meanwhile, simply cutting back on total calories is fraught with peril as well. An excellent study by Harvard University researchers confirms that the kinds of foods one eats — rather than total calories per se — is the most important indicator of whether a given eating pattern leads to weight gain or loss.
So what’s the best way of eating to manage weight? Fortunately, some answers are emerging.
Increasingly, chronic, inappropriate inflammation is widely recognized as a driver of obesity. Inflammation in the body is a normal and healthy response to injury or attack by germs. We can see it, feel it and measure it on the surface as local heat, redness, swelling, and pain. This is the body’s way of getting more nourishment and more immune activity into an area that needs to fend off infection or heal. But whole-body, elevated inflammation — as evidenced by increased levels of certain protein markers in the blood — has actually been shown to predict future weight gain in a study of non-diabetic healthy men. Inflammation, in short, helps make you fat.
Obesity, in turn, promotes chronically elevated inflammation. As this Harvard review article puts it, “A chronic, subacute state of inflammation often accompanies the accumulation of excess lipid in adipose tissue and liver (hepatic steatosis), evidenced by changes in both inflammatory cells and biochemical markers of inflammation.”
In other words, obesity and inflammation feed each other in a destructive cycle. This may help explain why weight, once gained, can be so difficult to lose.
Which brings me to a fascinating new paper by Ian Spreadbury of the Gastrointestinal Diseases Research Unit at Queen’s University in Ontario, Canada. It provides what I believe could — and probably should — become the dominant index for deciding which foods to eat and which to avoid in pursuit of weight control. Bearing the daunting title, “Comparison with ancestral diets suggests dense acellular carbohydrates promote an inflammatory microbiota, and may be the primary dietary cause of leptin resistance and obesity,” the paper lays out the hypothesis that carbohydrate density is probably the most important determinant of whether a food promotes inflammation/obesity or not.
Carbohydrate density is simple to calculate — just divide the quantity of carbohydrate in food by the weight of the food. The more carbs that are packed into a given gram of food, the higher its carbohydrate density.
Modern food processing is, unfortunately, very good at boosting carbohydrate density. Two of the most powerful ways to do it are isolating and concentrating sugars from plants, and grinding dense seeds into highly compactible flour. In both cases, heat and pressure damage or obliterate the original food’s cell walls. To use Spreadbury’s terminology, sugar and flour are acellular — almost wholly lacking in intact cells.
According to Spreadbury’s review, these carbohydrate-dense, acellular foods may help to make the normal, natural bacteria that inhabit the digestive tract become pro-inflammatory. One destructive consequence: these inflammation-promoting microbes produce “leptin resistance in vagal afferent endings”; in other words, a blunting of the ability of leptin and other hormones that say “I’ve eaten enough” to communicate that message to the brain via nerve endings in the gut.
This matters, as virtually every physician who counsels obese patients hears the refrain, “I just never feel full!” Such complaints should not be dismissed as fanciful — it’s quite possible that people with inflamed GI tracts really do wrestle with more or less continuous, unquenchable feelings of hunger, making weight loss far more difficult than it should be.
If Spreadbury is right, the obesity solution is straightforward. I’ll discuss that, and list specific high- and low-density carbohydrate foods, in “Using the Carbohydrate Density Index.”
Andrew Weil, M.D., is the founder and director of the Arizona Center for Integrative Medicine and the editorial director of www.DrWeil.com. Become a fan on Facebook, follow Dr. Weil on Twitter, and check out his Daily Health Tips Blog.