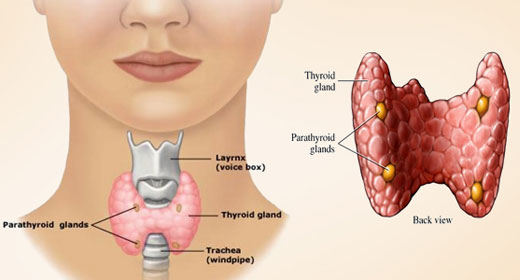
The butterfly-shaped valve in the neck known as the thyroid gland, might be small, but it plays a big part in how your body works.
It contributes to your metabolism, your body’s temperature, and even your heartbeat. An underactive or overactive thyroid can cause you problems that you are not even aware of. There are other conditions that are more serious that are associated with the thyroid. If you find yourself with any of the following eight symptoms, then it’s a good idea to get your thyroid checked by your doctor.
1. You are more tired than usual
There are many reasons why you could be suffering from fatigue but one of which, could be an over or underactive thyroid. So if you are getting a good night sleep but are still feeling tired and can’t think of any other reasons for what you are experiencing, this could be the underlying cause. Exploring this further by visiting a trusted medical professional is recommended.
2. You have a hoarse throat
Constantly feeling sore in your throat or sounding hoarse when you speak, might be down to your thyroid. When your thyroid isn’t working as it should be, it goes into overdrive, and this can cause inflammation and swelling in the throat. You might even physically notice a lump or your throat just looking bigger than usual.
3. Forgetfulness
We all get a little forgetful sometimes, but if it’s happening more often than what it should, this could be down to your thyroid. Lacking concentration, forgetfulness and feeling quite blank are all signs that are associated with hyperthyroidism. Getting treatment for your thyroid problem should help keep your mind fog at bay and have you feeling like yourself again in no time.
4. You always feel cold
Many thyroid conditions result in you being unable to control your body temperature. This makes you feel cold all the time. If you are wearing two sweaters, you’ve turned up the thermostat, and you STILL feel cold, it’s worth going to see your doctor and check if your thyroid is the culprit.
5. You’ve gained weight
Your thyroid is what helps control metabolism so when it isn’t working properly, your metabolism will slow down which will make you burn fewer calories. This can result in unexpected weight gain even if your eating habits or levels of exercise have not changed in any way. Losing sudden weight can also be an issue of thyroid problems although this is less common than gaining weight.
6. Your heart is racing
Having a racing heart rate is something that can be worrying, but it could have something to do with your thyroid, and this is something that is hopefully easy to treat after you’ve gone to your doctor. Research by Harvard Health Publication has said that a racing heart could be a symptom of an overactive thyroid or your thyroid producing too many hormones in your bloodstream to handle.
7. Fertility issues
If you are a woman who is struggling to get pregnant, the problem could be an unsuspected one – your thyroid. Women for Women have discovered that thyroid issues can lead to an irregular menstrual cycle which can complicate for you to get pregnant, due to not being able to track ovulation effectively. If you are a man who has a thyroid problem, it can result in your testosterone levels to drop which can cause fertility problems as well.
8. Stiff or swollen joints
If you are suddenly experiencing weird feelings in your joints like soreness or stiffness that leaves you feeling uncomfortable, this could be due to an underactive thyroid. Research has shown that the condition could result in joint stiffness, pain, and swelling – the symptoms are said to echo the symptoms of arthritis. Swelling of the hands and feet can also be a sign of thyroid problems.
So What Should You Do?
Now you know some of the signs to look out for that indicate issues with your thyroid, you can decide as to whether you should get it checked out. You know your body so if something doesn’t feel right to you, go to a doctor. It’s always better to be safe than sorry because getting the right medication right away could significantly impact your life.
The thyroid gland is often described as a “butterfly-shaped” gland because it has two lobes that look like butterfly wings on either side of the trachea that are connected to each other by a central isthmus, which lies across the anterior portion of the neck (the front) at the base of the neck. It is only about two inches in length and about an inch in height, making it the size of a large butterfly and often difficult to feel unless it is enlarged. Not everyone has an isthmus.
The thyroid gland lies just beneath the thyroid cartilage, which in males is known as the “Adam’s apple”. Its main function is to control the metabolism of the cells the body. It is a typical endocrine gland, meaning that its function is mediated by the release of hormones into the bloodstream that act on distant sites of the body. The two main thyroid hormones released by the thyroid gland include thyroxine (T4) and triiodothyronine (T3).
The levels of T4 and T3 are tightly regulated in the body as too much or too little of the hormones will cause symptoms connected to an imbalance in the body’s metabolism. Both the hypothalamus in the brain and the pituitary gland, located beneath the brain near the hypothalamus, are responsible for the amount of T3 and T4 that are released via a feedback loop—something very common in the endocrine system.
The thyroid feedback loop looks like this: The hypothalamus makes thyrotropin-releasing hormone or TRH into the hypothalamic-pituitary portal, which connects the hypothalamus to the pituitary gland. This triggers the anterior pituitary gland to release thyroid stimulating hormone or TSH. TSH carries the signal to the thyroid gland and binds to TSH receptors on the cells of the gland. The binding of the receptor causes T3 and T4 to be released. When the levels are too high, a signal is sent to the hypothalamus, telling it to turn off production of TRH. TSH levels fall and so do the thyroid hormone levels.
The thyroid hormones are crucial to every cell of the body by regulating the speed of cellular metabolism. In the intestinal tract, they control how quickly food is digested. In the heart, they control how fast the heart beats and how strong the muscle cells are. They regulate the speed of nerve cells. This is why an underactive thyroid gland can lead to a slow heartbeat, weight gain, and constipation. An overactive thyroid gland, on the other hand, may cause tachycardia, anxiety, and diarrhea.
The metabolic processes that are directly affected by the thyroid gland and its hormones include body weight, muscle strength, cholesterol levels, gastrointestinal motility, brain function, peripheral nervous system function, menstruation, body temperature, and heart rate. The symptoms of hypothyroidism involve an underactivity of these bodily functions while the symptoms of hyperthyroidism involve an overactivity of these bodily functions.
TESTING THYROID FUNCTION
Thyroid function testing primarily involves performing blood work. In general, the true picture of thyroid function cannot be gotten by a single test. It usually takes at least two tests of different hormone types to assess the hypothalamic-pituitary-thyroid axis. Just one test, like the T3 level, can mean that the thyroid gland is dysfunctional or that the pituitary gland is not making enough stimulatory TSH. It doesn’t say enough about the total picture. A low TSH level, along the same lines, can mean there is dysfunction of the hypothalamus or the pituitary gland. It can also mean that the thyroid gland is overproducing T4 and T3, resulting in a negative feedback loop and low TSH levels.
A low T4 level and a low or normal TSH level means that the pituitary gland is not responding to the low T4 level. As the hypothalamus is rarely damaged, the problem is most likely with the anterior pituitary gland. Pituitary gland failure is extremely important to diagnose because this is a gland that acts on many other endocrine glands and cells of the body, while thyroid gland failure alone just affects the metabolism.
Typical tests used to evaluate the thyroid gland function include the following:
- T4 test—this test is done using a radioimmunoassay technique and detects the level of thyroxine in the blood (both bound to thyroglobulin and free T4). It is a fairly good representation of the thyroid function. T4 represents 80 percent of all thyroid hormone released.
- T3 test—this is also done using a radioimmunoassay technique and detects the T3 levels, which represents 20 percent of thyroid hormone released. It can help to test for T4 along with the T3 level as an initially diseased thyroid gland may pour out T3 into the bloodstream just before it is going to fail and a normal to low T4 level at the same time may be able to diagnose this problem.
- TBG level—TBG stands for thyroid binding globulin, which is the blood plasma protein that binds thyroid hormones during their transportation from the blood to the cells. A deficiency of TBG or an excess of the hormone may artificially raise or lower T4 and T3 levels in the total but not the free T4 and T3 levels. If the elevation or reduction in thyroid hormone levels don’t match with symptoms, the TBG level can be drawn to shed some light on the free levels of these hormones.
- TSH test—this is a common thyroid test that measures the amount of thyroid simulating hormone in the bloodstream. An elevated TSH level generally means that the thyroid gland is not working and the pituitary gland is responding by making extra TSH to compensate for this. A low TSH level can mean that the pituitary gland is dysfunctional or that the thyroid hormones are high, signaling the anterior pituitary gland to shut off TSH production. An elevated TSH is often the first sign of impending thyroid disease.
- TRH test—this is not commonly done but is technically one of the available tests. TRH (thyrotropin releasing hormone) is injected into the bloodstream. Patients with an excess of thyroid hormones will not demonstrate a rise in TSH when TRH is given, while people with hypothyroidism will have an exaggerated TSH rise after giving TRH. This test is generally unnecessary as the sensitive TSH test can easily detect low and high thyroid conditions.
- Iodine uptake scan—this is a radioactive iodine uptake test. The patient is given radioactive iodine, the mineral that is preferentially taken up by the thyroid gland in order to make iodine containing-thyroid hormone molecules. The amount of radioactive iodine taken up by the thyroid gland is measured in this test.
- Thyroid scan—this is the actual picture of the thyroid gland after injecting radioactive iodine. A nuclear scanner can detect the thyroid gland function by highlighting those areas where the thyroid gland is taking up the radioactivity. It can detect “cold nodules” that are areas on the thyroid gland not taking up the radioactive iodine. It can also detect “hot nodules” or diffuse uptake in parts of the thyroid gland that are taking up too much radioactive iodine.
- Thyroid ultrasound—this makes use of sound waves directed at the thyroid gland in the neck. It can identify nodules and enlargement of the thyroid gland. It can tell if the nodules in the thyroid gland are solid or cystic but can’t always tell the difference between a cancerous nodule and a non-cancerous nodule. It can, however, tell the provider where to direct a needle for a needle biopsy that can make the diagnosis.
- Thyroid antibody testing—this involves testing for the different types of autoantibodies that can be seen in Hashimoto thyroiditis and Graves’ disease. Both of these diseases will have autoantibodies that can be assessed in these diseases. The main autoantibodies that can be assayed for include the thyroid peroxidase antibody (TPO) (for Graves’ disease or Hashimoto thyroiditis), thyroglobulin autoantibody (TGAb), thyroid stimulating immunoglobulin (TSI) (which is a test for hyperthyroidism), and thyroid binding inhibitory antibody (TBII) (which is a test for hypothyroidism).
- Thyroid needle biopsy—this is a test that can detect cancerous nodules versus benign nodules of the thyroid gland. A needle is inserted into the nodule under ultrasound guidance with the ability to identify the pathology of the nodule 75 percent of the time. If it fails, a repeat test could be performed or a surgical biopsy is obtained in order to define the underlying pathology in the thyroid gland.
THYROID DISORDERS
In this section, we will talk about the most common thyroid disorders, including goiter, thyroid nodules, hypothyroidism, hyperthyroidism, Hashimoto thyroiditis (and less common types of thyroiditis), and thyroid cancer.
GOITERS
The term, goiter, refers to a significant enlargement of the thyroid gland. Goiters tend not to be cancerous and often don’t release a great deal of thyroid hormone, only being removed because of the tendency of goiters to press on nerves or the trachea, because they interfere with swallowing, or because they are cosmetically unappealing. Goiters can be smooth or “multinodular”—having many nodules that collectively lead to an enlarged thyroid gland. No one knows the incidence of goiter as most of them arise in developing countries.
People with goiters can have normal thyroid function (called being euthyroid), hyperactivity of the thyroid gland (called being hyperthyroid), or hypoactivity of the thyroid gland (called being hypothyroid). Symptoms of hyperthyroidism include weight loss, tachycardia (rapid heartbeat), diarrhea, and anxiety. Symptoms of hypothyroidism include weight gain, slow heartbeat, constipation, tiredness, and depression.
There are several causes of a goiter. In developing countries that have no access to iodized salt or ocean fish, a goiter can be caused by a deficiency of iodine. This leads to an enlargement of the thyroid gland in an attempt to hold on to as much iodine as possible from the diet. It can be corrected by giving iodine. Graves’ disease can cause thyroid enlargement. In this disease, autoantibodies called “thyroid stimulating immunoglobulin” attack the thyroid gland. This results in an increase in the size of the gland and a goiter.
Patients with Hashimoto thyroiditis can also have a goiter. This is an autoimmune disease that makes antibodies that decrease T4/T3 output. The TSH from the pituitary gland is increased, stimulating an increase in the size of the thyroid gland. Multiple thyroid nodules and thyroiditis can cause inflammation or just swelling of the size of the gland. Less commonly, thyroid cancer can cause an enlargement of the thyroid gland.
There are treatment options for goiters. Those caused by iodine deficiency can be effectively treated with iodine supplementation, which causes a gradual decrease in the thyroid gland size. Patients with a goiter from Hashimoto thyroiditis can get improvement of their hypothyroidism by taking a thyroxine or triiodothyronine replacement drug, which is taken on a daily basis. Those who have hyperthyroidism and a goiter can be treated with radioactive iodine, which kills off the overactive cells, rendering the patient hypothyroid. Supplementation with T4/T3 is often recommended after that. Rarely, a partial thyroidectomy can be done to reduce the bulk of a goiter.
THYROID CANCER
Thyroid cancer is a relatively common type of cancer, with about 1.2 percent of individuals being diagnosed with thyroid cancer at some point during their lives (and a male to female ratio of 1:3). The vast majority of thyroid cancers are papillary thyroid cancer. While cancer can happen to anyone, it is most common in individuals 30 years of age or older.
Thyroid cancer is frequently asymptomatic in the beginning. The most common early finding is that of a lump in the throat area or rarely, a change in voice or hoarse speech. Only medullary cancer tends to be painful in the early stages as it can inflame the healthy thyroid gland tissue. About 1 percent of thyroid nodules are cancerous, found during a routine physical exam or CT scans obtained for reasons other than thyroid disease.
There are four main types of thyroid cancer. As mentioned, papillary thyroid cancer (or a mixed cancer with papillary and follicular features) comprise about 85 percent of cancers. Hurthle cell cancer or follicular thyroid cancer makes up 10 percent of cancers of the thyroid gland. Medullary thyroid cancer makes up about 3 percent of thyroid cancers, and anaplastic thyroid cancer accounts for 1 percent of thyroid cancers.
Papillary thyroid cancer comes out of an overgrowth of cancerous tissue in otherwise normal thyroid gland tissue. It is usually found between thirty and fifty years of age and is seen three times more often in females. It is sometimes caused by radiation exposure to the neck and spreads to the lymph nodes half the time. Distant metastatic spread generally does not occur with an overall cure rate of almost 100 percent in young people without metastatic disease.
The ten-year survival rate for people with papillary thyroid cancer is about 80-90 percent. While lymph node metastases do increase the risk of recurrences, these can easily be treated so that the mortality rate is no different than with non-metastatic disease. If distant metastases do occur, they tend to be located in the bones or lungs.
Follicular thyroid cancer tends to happen in older individuals and doesn’t arise from radiation to the neck. The mean age at onset is 40-60 years of age with a three-fold increase in incidence among women compared to men. Spreading to lymph nodes is not common (at about 10 percent of this type of cancer); however, local invasion is more common than with other cancer types. Because it happens in older people, the prognosis is worse when compared to papillary cancer. Metastatic disease to lung and bone are more common than with papillary cancer. Even so, about 95 percent of patients can be cured.
Medullary thyroid cancer arises from the C cells of the thyroid that make calcitonin. It tends to be more prevalent in females and easily spreads to cervical lymph nodes; it can frequently metastasize to places like the adrenal medulla, brain, bone, and liver. It isn’t linked to radiation exposure and can be part of multiple endocrine neoplasia IIB syndrome. When part of an MEN syndrome, the cancer has a worsened prognosis and it tends to be worse in older patients. The 10-year survival rate is about 90 percent with confined disease, 70 percent with lymphatic spread disease, and 20 percent with metastatic disease.
Anaplastic thyroid cancer is the least common type of cancer and the one with the poorest prognosis, having a survival rate of less than one year in most cases and an extremely poor cure rate. It tends to be seen in individuals who are more than 65 years of age and has a 2:1 male: female ratio with regard to incidence. It grows rapidly and can be secondary to previous radiation exposure for other reasons. Lymphatic spread is seen in 90 percent of patients at the time of diagnosis, and metastatic cancer to bones or the lungs are common. It can arise from a previously differentiated cancer or from normal thyroid tissue. Tracheal encroachment happens a fourth of the time, necessitating the placement of a tracheostomy tube for breathing. The three-year survival rate is less than ten percent, even with aggressive treatment.
THYROID NODULES
Thyroid nodules can be isolated or clustered with many nodules in otherwise normal thyroid tissue. As many as 90 percent of individuals aged 80 years or older will have at least one thyroid nodule. They often are cystic and this means they aren’t cancerous. In other cases, they are solid and may look like cancerous nodules. In such cases, the nodules are biopsied with a fine needle aspirate biopsy done under ultrasound guidance.
Most thyroid nodules are asymptomatic in that they don’t produce any thyroid hormones. Some nodules are called “hot nodules”, making T3 or T4 and having the same symptoms as hyperthyroidism, including rapid heartbeat, heat sensitivity, irritability, anxiety, diarrhea, tremor, weight loss, oligomenorrhea (infrequent periods), and hair loss. Other nodules are “cold nodules” and don’t make any thyroid hormones.
No one knows the exact cause of thyroid nodules. They may be hereditary, as they tend to run in families and they may be metabolic, as they are seen in iodine deficiency. Cancerous changes in the thyroid gland are not a common cause of a thyroid nodule but it can happen. Females have a higher risk of thyroid nodules as do people with Hashimoto disease and prior radiation exposure.
Thyroid nodules can be identified by a clinical neck exam or by having a neck CT or ultrasound for another reason. If the nodule is suspicious for cancer, it can be biopsied with fine needle aspiration. To see if a nodule is one that is producing hormone, a TSH, T4, and T3 level can be drawn to check for hyperthyroidism. They tend not to need treatment unless they are symptomatic. Nodules resulting in hyperthyroidism can be managed with radioactive iodine treatments or injected alcohol ablation therapy. Rarely is surgical intervention necessary.
HYPERTHYROIDISM
Hyperthyroidism is defined as having too much thyroxine and/or triiodothyronine in the bloodstream—something that can be detected via a blood test. An overactive thyroid gland affects the metabolism and speeds the body processes so that things like weight loss, insomnia, sweating, tremor, rapid heart rate, and anxiety often occur. Patients with an elevated thyroid condition will have palpitations, mood swings, diarrhea, and diffuse muscle weakness as well. Women will have oligomenorrhea (irregular and infrequent periods) or light periods.
The most common underlying problem causing hyperthyroidism is Graves’ disease—an autoimmune disorder in which autoantibodies are made called thyroid stimulating immunoglobulin (TSI) that binds to TSH receptors, turning on the production of T4 and T3. This can be a hereditary disease, running primarily among women in a family. Another cause of hyperthyroidism is toxic nodular goiter or multinodular goiter. In this condition, the nodules themselves are the source of the hyperthyroidism. Viruses or immune system dysfunction can lead to thyroiditis and hyperthyroidism. Excessive iodine consumption or the consumption of drugs containing iodine can lead to hyperthyroidism. There is an uncommon condition of hyperthyroidism associated with pregnancy or having given birth.
The diagnosis of hyperthyroidism depends on the identification of the symptoms of the disease and on confirmatory blood testing. If the blood tests are consistent with hyperthyroidism, an ultrasound or nuclear scan (using radiation) can identify nodules that are excessively producing thyroid hormone. Diffusely increased activity of the thyroid gland can also happen and will be seen on a nuclear scan.
Hyperthyroidism is generally treated initially with anti-thyroid medications, such as propylthiouracil and methimazole. These are often given temporarily until definitive treatment is given. Definitive treatment usually means giving high doses of radioactive iodine. The thyroid gland preferentially takes up the radioactive material, which kills the thyroid tissue it attaches to. Beta-blocker drugs can reduce some of the symptoms before definitive treatment can be given.
HYPOTHYROIDISM
Hypothyroidism involves having a deficiency of T4 and/or T3 in the body. It is the most common disorder of the thyroid gland, often being initially a silent disease. There are about 10 million people in the US with hypothyroidism and some report that the incidence of hypothyroidism in women is as much as 10 percent. These patients will have symptoms associated with low metabolism.
The main causes of hypothyroidism include inflammation of the thyroid that ultimately kills the cells of the gland, leading to a low thyroid state. The most common thyroiditis is Hashimoto thyroiditis, an autoimmune disease in which autoantibodies are made against the thyroid gland tissue, causing an immune destruction of the gland. The only other major cause of hypothyroidism is the surgical removal or destruction of the thyroid for other reasons. Thyroid cancer treatment can lead to secondary hypothyroidism by removing too much thyroid tissue. Goiter removal can contribute to thyroid dysfunction later. Radioactive iodine treatment for hyperthyroidism also leads to secondary hypothyroidism. Rarely, the failure of the pituitary gland can lead to a hypothyroid state.
Typical symptoms of hypothyroidism include hair loss, dry skin, dry hair, weight gain, constipation, overall weakness, tiredness, intolerance to cold, muscle cramping, decreased sex drive, frequent menstrual periods, memory loss, irritability, and major depression. In mild cases, just a few symptoms can be present with an increase in the number and severity of the symptoms as the disease worsens. The thyroid gland can enlarge into a goiter if the TSH level from the pituitary gland is so high that it overstimulates the thyroid gland. Severe hypothyroidism can lead to suicidality, heart failure, coma, and death.
The treatment of hypothyroidism is to replace the thyroid hormone with an exogenous pill that is taken every day. The pill contains thyroxine and sometimes triiodothyronine. There are many different preparations and dosages to take, with the dose titrated so the TSH is within normal limits, indicating that enough hormone is feeding back to the pituitary gland so it doesn’t need to put out stimulating hormone.
The most common treatment for hypothyroidism is levothyroxine, a synthetic form of T4. It comes in a variety of strengths and the dose is adjusted according to symptoms and the blood thyroid hormone levels. Frequent dosage adjustments may need to take place in the beginning of the treatment. The hormone levels are checked after the first month of starting the drug and periodically after that to make sure the T4 and TSH levels remain normal.
THYROIDITIS
Thyroiditis is defined as any inflammation of the thyroid gland. It can be an asymptomatic disease, or can present with hypothyroidism or hyperthyroidism. Some patients will have inflammatory symptoms, such as fever or localized neck pain. There are a few types of thyroiditis with most of them being extremely uncommon.
The most common type of thyroiditis is called Hashimoto thyroiditis, named after the researcher who discovered the disease. It represents the most common thyroid disease in the US and is also referred to as autoimmune thyroiditis or chronic lymphocytic thyroiditis. The body makes anti-thyroid antibodies that bind to thyroid tissue, initiating an immune response that inflames and eventually destroys normal thyroid tissue. It is seven times more likely to occur in women when compared to men. The main outcome of this is hypothyroidism. The inflammation of the gland can also lead to a goiter. The main treatment for Hashimoto thyroiditis is to replace the thyroid hormone no longer made by the thyroid gland.
Hashimoto thyroiditis is often entirely asymptomatic in the early stages of the disease. The main symptoms, when they appear, include those related to being hypothyroid and those from having a goiter. Goiters with this disease can be painful or just uncomfortable from the swelling of the neck. Large goiters can interfere with a person’s ability to breathe and swallow properly. Typical hypothyroid symptoms can develop as part of having this type of thyroiditis.
The main risk factors for developing Hashimoto thyroiditis is having another autoimmune disorder (as they tend to cluster together in the same person). Patients with autoimmune diseases have some type of impairment of their immune system that results in the frequent development of autoantibodies to various body tissues, including the possibility of thyroid tissue-directed antibodies. People with autoimmune disorders (such as type 1 diabetes, rheumatoid arthritis, or Crohn’s disease) should have a periodic assessment of their thyroid function to check for Hashimoto thyroiditis.
The three main tests for Hashimoto thyroiditis include a serum TSH level, which assesses the function of the pituitary gland and its ability to react to low T3/T4 levels. This is perhaps the most sensitive test of thyroid dysfunction in Hashimoto thyroiditis, although it can be elevated in other types of low thyroid conditions. Elevated TSH levels indicate a decreased concentration of either T3 or T4 in the blood with feedback to the hypothalamus and pituitary gland telling them to put out compensatory hormones in an attempt to raise the failing thyroid hormone levels.
Anti-thyroid antibody testing is very specific for Hashimoto disease and won’t be present in other types of thyroiditis or hypothyroidism. These include the anti-microsomal antibody level (also called the thyroid peroxidase antibody test) and the anti-thyroglobulin test (against the protein that carries thyroid hormone in the bloodstream). Either one of these autoantibodies can be positive in Hashimoto thyroiditis, leading to a reduction in the effectiveness or concentration of thyroid hormone in the body. The antibodies direct the immune system to kill off whatever is attached to them and, in these cases, the antibodies are attached to crucial parts of the thyroid gland function. Anti-thyroid antibodies will be positive 95 percent of the time in patients who have known Hashimoto disease. The levels will be elevated even as the disease is treated because there is no treatment for the autoantibody elevation.
A free T4 test can be done to evaluate the amount of thyroid hormone in the bloodstream and, while not specific for Hashimoto thyroiditis, will be decreased in the disease and will be a good confirmatory test. It is best interpreted in light of also doing a TSH level as well, which can show the classic pairing of the high TSH level and low T4 level typical of hypothyroid states, including that seen in Hashimoto disease. In very mild disease, there can be an elevation of TSH with a normal T4, as the TSH is stimulating the thyroid gland to make as much hormone as possible. As the disease progresses, the T4 level eventually falls.
In testing for Hashimoto thyroiditis, a nuclear scan with radioactive iodine may show an increased uptake, particularly in the early stages. The thyroid gland will be enlarged as a way to compensate for a failing thyroid gland and the thyroid still has the ability to trap iodine molecules, resulting in a paradoxically elevated uptake of the radioactive iodine. As the disease worsens, this ability to bind iodine goes down and the radioactive iodine uptake levels will be low.
DeQuervain’s thyroiditis is a less common type of thyroiditis when compared to Hashimoto disease. It is also referred to as granulomatous thyroiditis or subacute thyroiditis. It results in extreme swelling of the thyroid gland,a associated with thyroid pain and tenderness as major symptoms of the disorder. These patients will become markedly hyperthyroid with symptoms of hyperthyroidism until the gland eventually stops taking up any type of iodine, leading to a resolution of the hyperthyroidism over a few weeks.
Patient with DeQuervain’s thyroiditis tend to be very ill and will have coexisting malaise and fever. The disease acts like an infectious process but no infectious agent can be found as the cause of the thyroiditis and taking antibiotics will not help the disease process. Patients may get better with corticosteroids and sometimes the provision of thyroid hormone, which allows the thyroid gland to put out less of its own thyroxine and triiodothyronine, providing a rest period for the inflamed gland. Some patients will become hypothyroid from burn out of the thyroid gland and will need lifelong replacement of thyroid hormones. Most patients, however, will recover completely without adverse sequelae.
Silent thyroiditis is the least likely cause of thyroiditis and the most difficult to diagnose. It has clinical similarities to Hashimoto thyroiditis and DeQuervain’s thyroiditis. Unlike DeQuervain’s disease, the thyroid gland is not painful and, if a needle biopsy is obtained, it will closely resemble Hashimoto disease. There is a predominance of females with the disease and it usually affects young people.
There is no recommended treatment for silent thyroiditis and more than 80 percent of sufferers will recover completely within a few months. The amount of radioactive uptake during the active phase of the inflammation will be low but will return to normal after the disease regresses. The thyroid gland is usually minimally enlarged and the symptoms resemble those of Graves’ disease.
The treatment of choice for silent thyroiditis is to provide the patient with beta-blockers to control hyperthyroid symptoms. There is no other treatment necessary and treatment with things like anti-thyroid drugs, surgical excision, or radioactive iodine only destroys or damages a thyroid gland that will otherwise completely recover without any more treatment necessary other than to treat the symptoms. Some patients will, however, burn out their thyroid gland, resulting in a permanently hypothyroid state.
ADDITIONAL RESOURCES
Hypothyroidism: The most common thyroid condition is hypothyroidism and it is covered thoroughly on this website. The information is geared toward family practice doctors but can be understood fairly easily by the well-versed layperson wanting to know the details of this low thyroid condition, the pathophysiology behind it, and the different treatment strategies used to manage this disorder.
Hyperthyroidism and Thyrotoxicosis: The phenomenon of the overactive thyroid gland and its extreme, thyrotoxicosis, are covered together in this comprehensive review of this relatively uncommon thyroid condition. This article focuses on the etiologies and pathophysiology behind hyperthyroidism, the ways in which healthcare providers evaluate the problem, and the ways in which both hypothyroidism and thyrotoxicosis are treated.
Hashimoto Thyroiditis: The most common type of thyroiditis is Hashimoto thyroiditis, which is an autoimmune type of thyroid disease. This is the topic of this review and includes the background of the disease, its etiology, its pathophysiology, medical workup, and treatment. This is an excellent site for anyone who has Hashimoto thyroiditis who wants to know what the latest information is on this common disease. The site is intended for healthcare providers but can be relatively easy to comprehend by laypeople.
Thyroid Cancer: This site begins with a discussion on the diagnosis of the isolated thyroid nodule and goes on to cover the major types of thyroid cancer. The pathophysiology of each of these thyroid cancers is covered along with the recommended treatments and therapies used to treat the different thyroid cancer types.
Goitier– The phenomenon of thyroid goiter has been identified in medical literature for several centuries, the modern approach to this uncommon thyroid problem is covered in a series of sections on this website. This is a good website for understanding the etiology of a goiter, how the underlying causes of the disorder are uncovered, and how a goiter is medically and surgically managed..
10 Signs You Have A Thyroid Problem And 10 Solutions For It: This is a basic overview of symptoms related to thyroid diseases and the different ways in which thyroid diseases are managed. This is a relatively basic site that will help the layperson understand the symptoms found in thyroid disease with simple explanations for the various symptoms. Its main focus is on the most common type of thyroid problem (hypothyroidism); it talks about some unconventional treatments for this condition.
19 Signs Your Thyroid Isn’t Working Right: This is a website that primarily covers the different symptoms that are associated with hypothyroidism, the most common of the thyroid disorders. It covers 19 different symptoms that can be linked to this disorder in detail and is a good site for someone who suspects they might have hypothyroidism but isn’t sure they have the right symptoms. This might be the easiest site to go to for questions about the symptoms involved in low thyroid conditions.