by Ocean Robbins: When medical researchers encountered the Pima tribe of Southern Arizona in the early 1960s, they were astounded at their poor health…
We are proud to announce a new partnership with John and Ocean Robbins and the Food Revolution to bring our readers Summits, Seminars and Masterclasses on health, nutrition and Earth-Conscious living.
Sign Up Today For the Healthy Brain Masterclass
Obesity was rampant, and close to 50% of residents 35 and older had type 2 diabetes — by far a world record.
You might be thinking there must be some pretty bad genes in play there. But thanks to the geopolitical factors that created the US-Mexico border, the real story is very different.
After US surveyors drew their maps following the Mexican-American War of 1849, part of that same US-based Pima tribe ended up in the highlands of Mexico. Genetically, the two groups are extremely similar, which is what you’d expect since they’ve been separated only for a couple of centuries. But here’s the kicker — the Mexican Pima experience just one-fifth the incidence of diabetes of their American counterparts.
If it’s not the genes, then what is it? According to researchers, the answer lies in the two communities’ very different lifestyles. And topping the list of lifestyle factors were physical activity and diet. The Mexican Pima, similar to their non-Pima neighbors, got a lot more exercise and ate a much less processed diet — far lower in fat and higher in fiber — than the Pima in Arizona.
Whether you are trying to avoid developing type 2 diabetes, or you’ve already got it and are trying to manage it effectively, living more like the Mexican Pima and less like the American Pima is a useful strategy.
In this article, we’ll explore what to eat for type 2 diabetes, including nine foods that are exceptionally powerful in helping maintain healthy blood sugar levels.
The Diabetes Epidemic
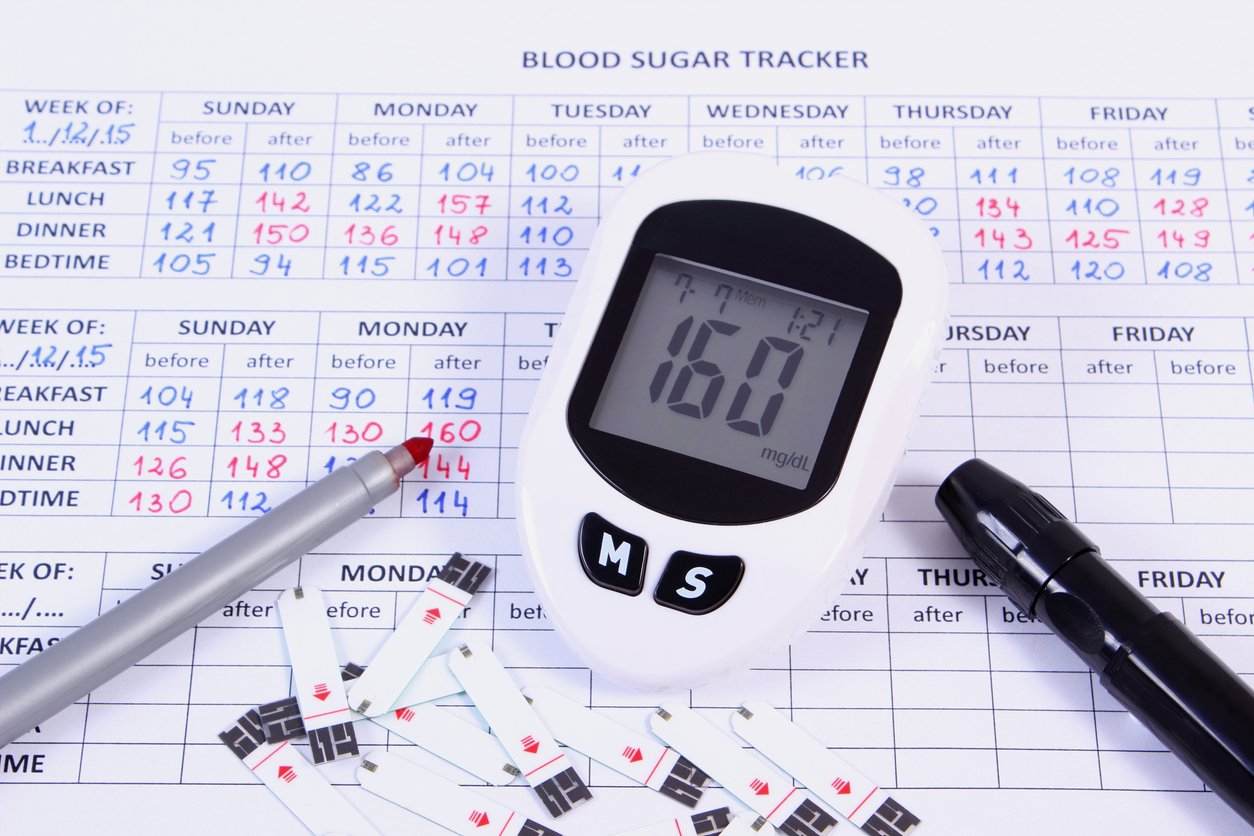
Type 2 diabetes is defined by excess glucose in the blood, and is typically diagnosed when a person’s A1c (a 3-month average blood sugar level) is 6.5% or higher, or when their fasting blood plasma glucose reaches 126 mg/dl or higher.
Rates of type 2 diabetes have been steadily rising for several decades. In the US, the prevalence of type 2 diabetes among US adults increased from 10% in 2001 to almost 15% in 2020. It wasn’t one particular cohort that was affected — similar trends emerged from all categories examined, including age, sex, racial and ethnic group, and education level.
Globally, an estimated 462 million people are affected by type 2 diabetes, making up more than 6% of the world’s population. And many more people worldwide suffer from prediabetes, which indicates an impaired glucose tolerance (and is diagnosed when A1c is between 5.7% and 6.4% or fasting plasma glucose is between 100 and 125 mg/dl). The incidence of prediabetes was estimated at an additional 7.3% of the world adult population in 2017, equivalent to over 350 million people.
What Causes Type 2 Diabetes?
While you have a better chance of developing type 2 diabetes if a parent or sibling also has it, your genes are not the main predictor, as we saw with the Pima. Even if you have genes that predispose you to diabetes, it’s your diet and lifestyle that tend to turn those genes on or off. Type 2 diabetes is therefore defined as a lifestyle disease, primarily caused by underactivity and being overweight or obese.
Since type 2 diabetes often (but not always) corresponds with being overweight or obese, two of the most powerful factors that determine your risk are energy intake and expenditure — how many calories you consume, and how many you burn. Which means that diet plays a major part in the development and maintenance of the disease (as well as its precursor, prediabetes).
The thing that determines how well your body transports glucose from your blood into the tissues where it’s needed (like your muscles, liver, and fat cells) is called insulin tolerance. Insulin is the hormone that acts like a key, opening your cells to let in glucose. If your tissues become resistant to insulin’s “key,” and stay shut even in the presence of high levels of blood glucose, that’s known as insulin resistance.
Insulin resistance can develop due to a number of factors, including being overweight, underactive, or eating a diet rich in sugars and fats. That is to say, the standard American diet — high in processed foods, refined sugar, and animal products — contributes to the incidence of type 2 diabetes. Which begs the question: If the way many people are eating is causing or progressing the disease, how do you know what to eat for type 2 diabetes? What diet is best? And what are the specific foods that are best for helping tackle type 2 diabetes?
Is Eating Low-Carb for Diabetes Healthy?

Since diabetes is defined as excessive blood sugar, wouldn’t it make sense to prevent or deal with the condition by eating a low-carb diet? After all, carbohydrates turn into sugar in your body, which is how they’re used for energy. You might think, therefore, that sugar causes type 2 diabetes by triggering spikes in blood sugar.
That was the standard mainstream approach for many years. But we’ve discovered that there’s a lot more to the story than just eliminating carbs and sugar. First of all, not all carbohydrates act the same way in the body. And not all carbohydrates cause type 2 diabetes or make it worse.
Fiber is a type of carbohydrate, but it actually helps slow the absorption of glucose while also regulating blood sugar over time. And there’s a big difference between simple carbs from white sugar and white flour and the complex carbohydrates in many whole, plant-based foods. Complex carbohydrates are generally better for you, often not spiking blood sugar thanks to fiber, water, and other buffering nutrients.
But here’s the crux of what we now understand about type 2 diabetes — high blood sugar is a symptom, not the cause. Which means that just eating sugar can’t be the sole root of the disease. It’s eating sugar in the presence of insulin resistance that creates the condition of type 2 diabetes.
Many things can lead to insulin resistance, including chronic inflammation, oxidative stress, and alterations in circulating lipids or fats. And animal foods can cause and exacerbate all three of these processes.
That’s why low-carb diets aren’t the answer. If you’re eating low-carb, you’re eating high-something else — either fat or protein. And if you’re consuming the standard American diet, either substitution generally means a diet high in animal products — which can cause insulin resistance.
What About the Keto Diet for Type 2 Diabetes?
That’s why keto diets, which may help in the short term with blood glucose levels and weight loss, are not sustainable. Because it’s so difficult to maintain such a severely reduced calorie consumption, keto offers a temporary Band-Aid rather than a true reversal of type 2 diabetes.
[Check out our article on the pros and cons of a keto diet.]
And keto tends to be high in saturated fat, which turns out to be one of the main drivers of insulin resistance. Saturated fat, which we predominantly get from eating animal products and tropical oils such as palm oil, can increase fat accumulation in cells and promote the formation of inflammatory compounds, both of which contribute to insulin resistance and type 2 diabetes.
The Best Diet for Type 2 Diabetes
So if low-carb and keto diets fall short, what is the best diet for preventing or managing type 2 diabetes? Here are some characteristics of such a diet:
- unrefined carbohydrates (vs refined carbohydrates),
- monounsaturated and polyunsaturated fats (vs saturated and trans fats),
- and plant protein (vs animal protein).
These dietary factors all play a major role in preventing and managing type 2 diabetes. And plant-based diets have all three of these characteristics.
Plant-based diets are the most effective for preventing and reversing type 2 diabetes and prediabetes. According to studies, the more calories you get from whole plant foods, such as legumes, veggies, fruits, nuts and seeds, and whole grains, and the fewer animal products, the lower your risk of developing type 2 diabetes.
Plant-based diets maximize dietary components that are protective against chronic disease, in general, and type 2 diabetes, in particular. These components include fiber, phytochemicals and antioxidants, and magnesium, all of which are found predominantly, if not exclusively, in plant-based foods.
Plant-based diets also minimize harmful dietary components that are found in meat and are linked to inflammation and insulin resistance, including TMAO, saturated fat, heme iron, nitrosamines, and AGEs.
A Science-Backed Diet for Diabetes
It’s not just theory, either: “Observational studies and randomized controlled trials support the benefits of plant-based nutrition for diabetes.” Three prospective cohort studies that followed over 200,000 US health professionals for up to several decades found that “plant-based diets, especially when rich in high-quality plant foods, are associated with substantially lower risk” of type 2 diabetes. Another study of almost 40,000 participants in rural China showed the same result. In the words of the researchers, “a higher score of the overall plant-based diet was associated with a lower risk of type 2 diabetes.”
In short, the consumption of whole grains, legumes, fruits, and vegetables in conjunction with the elimination of animal products reduces the risk of developing type 2 diabetes. And in people with type 2 diabetes, a low-fat, plant-based diet has been found to improve body weight, glycemic control, cholesterol, and blood pressure, while reducing the risk of heart disease.
Foods to Help Improve Insulin Resistance in Type 2 Diabetes
While a whole foods, plant-based diet is the most effective way of eating to prevent and manage type 2 diabetes, there are particular foods that have been shown to be especially effective in normalizing blood sugar. Here are nine of the foods that do the best job of decreasing insulin resistance, with two yummy recipes for each so you can add them to your diet right away.
1. Cinnamon

A 2019 meta-analysis of 16 randomized clinical trials found that cinnamon helps lower fasting blood glucose, although it doesn’t seem to impact the longer-term marker of blood sugar, A1c. The dosages were all over the place, from a single gram per day to as much as 14.4 grams per day, so it’s hard to say what an ideal dose might be. A 2020 study fed the experimental group 3 half-gram servings of cinnamon (which included cinnamon extract and Indonesian cinnamon) per day for 12 weeks and found that compared to controls, the cinnamon group had lower fasting plasma glucose. They also performed better on glucose tolerance tests.
Cinnamon appears to work via several mechanisms, including mimicking insulin and making it easier for your body to transport glucose from your blood to your muscle cells by slowing down the rate at which food leaves your stomach.
[For more on cinnamon and other healthy spices, see our article on healthy spices.]
Try these two cinnamon recipes for diabetes:
- Cinnamon Apple Breakfast Smoothie
- Gingerbread Granola
2. Beans
We know that people who eat beans regularly are less likely to develop prediabetes than bean avoiders. A 2012 study out of Iran found that those who ate three or more servings of legumes per week had one-quarter the risk of metabolic syndrome (a condition closely linked to diabetes and prediabetes) than those who ate the fewest servings. Another study compared bean eating to caloric restriction. It found that when overweight and obese adults added five cups of lentils, chickpeas, split peas, or navy beans per week to their diet for eight weeks, they reduced their risk factors of metabolic syndrome as much as cutting 500 calories per day.
A 2018 prospective study out of Spain also looked at over 3,000 people’s diet and health statuses and found an inverse relationship between legume consumption and type 2 diabetes. That is, the more beans eaten, the lower the risk of diabetes.
What’s in beans that makes them so great for blood sugar control? There are so many beneficial compounds, it’s hard to know where to start. There’s the plant-based protein and soluble fiber, both of which are filling and prevent sugar spikes. There are polyunsaturated fatty acids, vitamins and minerals, as well as phytochemicals that are antioxidant and anti-inflammatory. And even some of the so-called “antinutrients” in beans may actually be nutritional heroes rather than villains, interfering with the metabolism of glucose.
Try these two bean recipes for type 2 diabetes prevention and management:
3. Apple Cider Vinegar

A 2019 study found that 20 ml (two-thirds of an ounce, or about 4 teaspoons) of apple cider vinegar (ACV) per day for eight weeks significantly lowered fasting blood glucose levels in people with type 2 diabetes.
Apple cider vinegar appears to work on both ends of the blood glucose puzzle: It can delay gastric emptying, which can prevent glucose spikes into the bloodstream. It also helps muscle cells utilize glucose, getting those sugars out of the bloodstream faster.
For more on apple cider and other types of vinegar, see our vinegar article.
Apple cider vinegar recipes to try for blood sugar control:
4. Low-Oxalate Leafy Greens
Some foods fight type 2 diabetes by focusing on a related issue, kidney health. Since your kidneys filter blood and remove waste products and excess fluid, when they aren’t working well, your blood glucose can rise to dangerous levels. And in a vicious cycle, diabetes can tax your kidneys to the point where they lose their ability to do their job — a condition known as chronic kidney disease.
Leafy greens, especially those low in oxalates (which can contribute to kidney stones), are great kidney boosters. These include kale, collards, arugula, lettuce, and many others.
A 2016 meta-analysis of 23 studies found that leafy greens are one of the categories of plant-based food most highly correlated with reduced risk of type 2 diabetes.
See our article on leafy greens for more info on how to source, store, wash, and prepare them.
Try these two leafy greens recipes for diabetes prevention:
5. Berries

Berries, including cranberries, strawberries, blueberries, blackberries, and raspberries, can decrease insulin resistance. And a 2016 meta-analysis found that eating blueberries reduced the risk of developing type 2 diabetes by 25%. Strawberries may also reduce oxidative and inflammatory stresses that can occur after eating.
Berries are rich in antioxidants called polyphenols, which come in different colors and account for the variety and intensity of the colors of the berries themselves. The red and purple hues come from anthocyanins, which are among the healthiest compounds you can get from plants.
Try these two diabetes-friendly berries recipes for breakfast or a snack:
6. Grapefruit
Grapefruit also appears on most lists of foods that combat type 2 diabetes. A 2021 review of large-scale prospective studies found that regular consumption of grapefruit reduced the risk of type 2 by about 10%.
One of the key components of grapefruit responsible for this effect may be the flavonoid naringenin — the average grapefruit contains about 100 mg of it. One study found that obese adults who ate three grapefruit halves a day for two to three months weighed less and had a smaller waist circumference than a control group.
Grapefruit recipes to try for blood sugar control:
7. Quinoa

Quinoa appears to earn its reputation as a superfood when it comes to preventing diabetes. A 2022 study out of Spain found that replacing other complex carbohydrates with quinoa reduced sugar spikes in older patients with prediabetes. Interestingly, participants were allowed into the study only if their existing diet was already pretty good and included grains, tubers, and/or legumes. The quinoa group had a better glycemic response to their meals, suggesting that quinoa could be effective in slowing the progression from prediabetes to full-blown diabetes even among relatively healthy eaters.
A 2022 test tube study suggests that it’s the polyphenols in quinoa that delay the digestion of starches. And indeed, when these polyphenols were isolated and fed to mice, the rodents displayed a muted glycemic response. (Our view on the use of animals in medical research is here.)
For more on this pseudocereal, read our in-depth quinoa article, here.
Try these two quinoa recipes for diabetes prevention and control:
8. Nigella Sativa or Black Seeds
Nigella sativa, also known as black seed (and sometimes black cumin seeds, but not to be confused with Bunium bulbocastanum black cumin seeds), has an impressive track record in combating type 2 diabetes. One 2010 study found that 2 grams per day of black seed over 12 weeks reduced fasting glucose as well as A1C in diabetic patients who were already taking antidiabetic meds.
A 2019 literature review identified seven studies confirming this finding, as well as observing an increase in serum insulin and a decrease in insulin resistance. And a 2021 article hypothesized the mechanisms by which black seeds might achieve these outcomes. If you get excited by phrases like “reduction of lipid peroxidation via its antioxidant properties,” “agonist of peroxisome proliferator-activated receptor gamma in adipose tissue,” and “activation of AMP-activated protein kinase,” then you will definitely want to add this article to your beach reading. For the rest of us, the basic takeaway is, “black seeds do a ton of stuff that appears to keep blood sugar under control.”
For more on cumin and black cumin, see our article here.
The benefits of black seed for diabetes can be experienced with these two delicious recipes:
9. Walnuts

While The Sopranos character Paulie Walnuts was dangerous, violent, and unpredictable, actual walnuts are one of the healthiest foods you can eat. And their ability to regulate blood sugar makes them great additions to your diet if you’re looking to prevent, reverse, or manage type 2 diabetes.
US survey data taken over the course of 15 years found that walnut eaters had about half the risk of type 2 diabetes as non-walnut eaters. And the association was dose-dependent, meaning the more walnuts, the lower the risk. A 2021 study from Spain identified 19 metabolites in walnuts that may contribute to the nuts’ ability to fend off type 2 diabetes, as well as heart disease. They include lipids, purines, acylcarnitines, and amino acids.
To see how you can use walnut for diabetes, try these two recipes:
The Best Foods for Type 2 Diabetes Are Plant-Based!
Diet is a major contributing factor in the development and progression of type 2 diabetes. Low-carb diets can keep your blood sugar low, but they may have unintended negative consequences. If you replace carbohydrates from disease-preventing foods — like vegetables, fruits, and whole grains — with animal products, you increase your long-term risk for chronic disease, including type 2 diabetes. And low-carb diets may not be sustainable for many people. Instead, you’ll likely be better off if you focus on eating a diet centered on nutrient-dense plant foods. And for extra protection, add generous portions of these nine plant-based foods that have been studied for their ability to help you tackle type 2 diabetes.











































