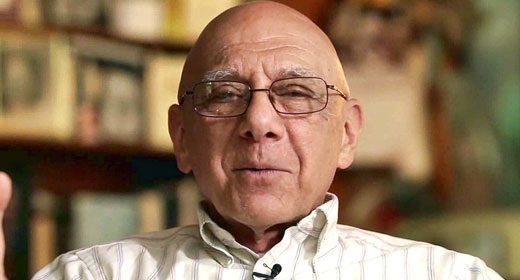
by Elaine Smookler and Patricia Rockman: In this podcast, Patricia Rockman, director of education and clinical services for the Center for Mindfulness Studies in Toronto, and…

Mindful columnist Elaine Smookler, both cancer survivors, talk about how mindfulness factors into the cancer experience.
What happens when the unthinkable happens to you? My name is Elaine Smookler, and I’m here in conversation with Dr. Patricia Rockman, co-founder and director of education and clinical services for the Centre for Mindfulness Studies in Toronto. Pat and I have been friends for decades and we were both training as clowns when Pat did, as her clown piece, a show called “From Birth to Death: It’s clown burlesque.” It was a life cycle show where the clown eventually began to lose body parts, bit by bit, as it went through the life cycle. Neither Pat or I knew at the time that this was going to be prescient for future experiences. Pat is here generously willing to talk about her experience with breast cancer and some of her insights about having gone through that process.
Elaine Smookler: Hi Pat, thanks for coming to talk with us today.
Patricia Rockman: Hi, Elaine.
Elaine: So I would love to know, What do you recall about your first moments after hearing your diagnosis of cancer?
Patricia: Well I already had a pretty good idea that I had breast cancer because I’d had some symptoms that made me suspicious. But getting the actual diagnosis —
Elaine: Do you want to tell us what those symptoms were just since you mentioned them?
Patricia: Mostly nipple crusting, which you can get when you do long runs and I had before but this was persistent so I was suspicious. So the diagnosis came on the phone from the pathologist and I really wasn’t surprised and at first didn’t feel anything at all. It wasn’t until they called my husband and spoke to him that I got really upset about it and we were both crying on the phone. So that was really my initial reaction.
Elaine: Very powerful. And you and your husband are physicians, so was there anything different do you feel — you’ve spent a lot of time with people who’ve also gone through cancer but who are your patients. What was that like for you and your husband being on the other side of it?
Patricia: Well there are some good things about being on the other side of it from the standpoint that I understand the system and I have a pretty good idea of how to make the medical system work best for me. On the other hand —
Elaine: And you have any tips for us when you say that, I mean that’s an interesting idea. Like what?
Patricia: Make sure that you ask a lot of questions, that you understand what’s going to happen in terms of the process. I think wheninv people are more informed they tend to do better. Also investigate: If you’re able to the research associated with the treatment that you’re having and if you feel the need to get a second opinion about what’s being suggested. Those are the main things.
If you have to have surgery, try to do your best to make sure that the surgeon is a good surgeon — this is not so easy to find out. It’s a lot easier to find that out when you work in the health care profession because invariably you will know somebody who knows somebody who works in OR, in an operating room, and this is what’s needed in order to really assess a surgeon’s skill because regardless of what people say about somebody it’s only when you see what they’re doing in that situation where you can really determine how good they are at their job.
Elaine: What’s interesting about that is that none of us may or not ever know the truth about that, but at least you have the understanding that you could ask those questions and do some investigation. I appreciate you mentioning it because it’s actually something that anybody could attempt to do. Certainly any of us are in position to ask questions and potentially, depending on your scenario, even change doctors if you’re not comfortable with the emotional support you’re receiving from your doctor because it’s a long journey and it’s good to know that you’re with the person who you feel you can talk to and connect with. Would you say that’s —?
Patricia: Somewhat. I think that with respect something like breast cancer where there may be a variety of treatments that you have to go through, not all breast cancers are treated in the same way. With something like chemotherapy or radiation there’s a protocol but when you’re working with a surgeon, not all surgeons are created equal. So you may think somebody has a really good reputation as a surgeon and they could be really bad. So it’s worth trying to find that out. As far as the emotional connection goes, I think for me working with the oncologist who provided the chemotherapy and was really the person who was at the head of the treatment team, having a connection with her was really helpful, really valuable. I wouldn’t say it’s so important with the surgeon. What I really care about in a surgeon is that they’re excellent with a knife.
Elaine: Okay fair enough! Alongside your experiences going through the physical components of cancer was the fact that you’re also a teacher, a writer, you’re the co-founder of the Centre for Mindfulness studies, so I’d like to know how did mindfulness factor in, how quickly did it come in. You talked about that first emotional experience with your husband. So what was the “and then what happened”?
Patricia: Change happens in an instant, every change happens in an instant. It tends not to be slow. Like the birth of a baby, you get married, you lose a job, you lose a spouse: These things happen quickly, it’s a psychological transition that takes time. I think mindfulness can help us with that because unless you’re incredibly evolved we’re always going to react to what life brings us. It’s really what you do next after that initial reaction — how might we respond skillfully or in a more healthy way.
Elaine: This is a really key point because I think for people who are just coming to mindfulness maybe particularly they’ve received a diagnosis of cancer their doctors said you should check out mindfulness. Perhaps they think mindfulness is going to solve all my problems and I really appreciate that you’re saying we’re still human beings. We’re going to have thoughts and feelings, they’re not always going to be peaceful.
If one expects one isn’t going to have difficult emotions, good luck with that. It’s what you do when they show up that matters: How do you treat yourself, how do you treat other people, what do you do next. Is it helpful or is it harmful?
—Patricia Rockman
Patricia: No. And in fact for me mindfulness has been most helpful in managing the difficulties of life. I often jokingly referred to myself as the queen of misery because I treat people with mental health problems who have depression and anxiety and people don’t come and see me because they’re happy. I really see my role as helping people to be able to manage difficult emotional and physical needs in healthier ways. Mindfulness can help us to be less immersed and overwhelmed by difficulty and be able to get a bit of space so that we can have choice about how we respond to what life throws at us. So for me, with the breast cancer experience, you’re immediately pitched into the role of a patient, you’re identified as sick even if you don’t feel sick. And treatment happens really fast with breast cancer. There isn’t a lot of time to contemplate, to think about, to adapt to the changing role. You’re kind of doing it all on the fly. I recognize in retrospect that there were certain decisions that I made from a reactive state, although I didn’t even necessarily know it initially so I ended up treating many decisions like they were urgent when in fact they were not. The only urgency is to start your treatment as quickly as possible. Whether that be chemo or whether that’s radiation or whether that’s surgery. All the rest can wait.
Elaine: So part of the mindfulness is the mindful awareness of our fight flight freeze response also of how quickly we want to get out of threat and how fast we might try to move away rather than giving ourselves the time and space. Is that what you’re saying to let it unfold a bit?
Patricia: Yeah. Mindfulness can help us to know when we need to do something and when we don’t. It can help us to see when we’re being driven by our emotional reactions and actually want to get away from the discomfort that comes with those versus when it’s actually necessary that we do something.
Elaine: So I’d like to investigate this a bit further. You used the word choice and there were some choice points in very kind of ordinary ways along the way that I would love to talk about. For instance some of the choices you had to make when your hair started to fall out.
Patricia: Right. It’s pretty much the norm, not everyone, but it is not uncommon that people will buy a wig when they lose their hair from chemo. Why is that? I didn’t even think about that initially. The health care provider I was seeing told me I should go and buy a wig and gave me some places to go check out. And I just dutifully went along and did that and it wasn’t until I was really into that process that I started to really think about like what am I doing here? Why am I doing this, this is incredibly unpleasant. The wig place is not able to match my hair. This is an agonizing process: I have to keep going back to this store when I’m feeling weak, and vulnerable, and sick. Ultimately they weren’t able to do what they said they could do and it was a bad decision to jump into that. There was no reason not to wait until my hair all fell out it and see, “How is this, being bald?,” can we bring beginner’s mind to baldness from chemo? In fact ultimately I chose not to buy a wig and had my head hennaed with a henna crown. It was beautiful. Motorcycle guys would stop me on the street and say how cool that tattoo was — of course it wasn’t really a permanent tattoo — but that being said it was lovely and being bold, I loved it, it was great.
Elaine: So when I think about how, If you open up Mindful magazine or you go to any website and look up mindfulness there’s so many different mindfulness practices a lot of them have a similar flavor but I feel you’re opening a whole door up here to a whole different kind of mindfulness practice that might come with mindfully deciding whether you really need to have a wig in order to be socially acceptable because you’re losing your hair during cancer because having gone with you during some of those wig processes I noticed that there were many thoughts and ideas that came up around acceptability, why do you need to have hair, what does that mean. And it was also powerful to notice what hair says about us. So the wig people believed the fact that they could give you something that covered your head that had an hairy quality to it was good enough. But as we looked in the mirror and saw the reflection back that didn’t look anything like the funky Pat that was in the world — What was the point of having a wig? And I felt that that really started to springboard the practice of noticing more deeply whose voices is it that’s calling us to do these things?
Patricia: It’s a cultural norm for women of hair for the most part unless you’re a punk rocker or something and hair is symbolic of many things: beauty, health. Wearing a wig, when you stop and think about it, is all about passing for being healthy, for being well, for not revealing that you’re sick, that it’s bad to be sick — just like the cultural message that it’s bad to be old. We hide these vulnerabilities away and it was really liberating to let go of that and also to make the decision to tell people. I remember when I was talking to my husband about it and one of the things that came up was I going to tell people that I have cancer. And he said well they’re going to know because your hair is going to fall out, which was pretty funny, and it made me stop and think: well why not let people know? We’re all going to get sick at some point or we’re all going to be exposed to people who are sick and we don’t get a lot of training in how to manage catastrophic illness or help others who are going through serious illness. And it became a way of normalizing that this is what happens to us and accepting that this is what’s here versus trying to avoid it. And for me that’s a big part of mindfulness as well.
Elaine: Beautiful. And you had other choice points that also showed up when you realized that you had to make some decisions about whether to have a prosthetic or not to have a prosthetic. Could you tell us a little bit about your decision-making and how you went about some of the events that came up around that?
Patricia: Well again I think that when we are pitched into these situations that are completely unfamiliar that are new, unknown, the outcome is unknown. We really try to control what’s going on, which doesn’t always work. And so one of the things that was on the table was whether or not I was going to have breast reconstruction, or implants, or nothing except a mastectomy. I initially thought I might go with nothing and had these imaginings of being an Amazon — the single breasted Amazons who would cut their breast off so that they could shoot their arrows more effectively and, yeah, nice thought except that I’m not an Amazon and I don’t have an arrow. And I also thought about that from a political perspective and ultimately made the decision to have reconstruction but this took a little while. I really was not in my right mind and was on the subway one day and saw this woman on the subway and looked at her. She was wearing an Indian shirt and I realized she only had one breast, which is something I would never have noticed if I wasn’t thinking about having a mastectomy. So I went up to her and asked her if she’d talk to me because I realize she only had one breast, which is a pretty strange thing to do with a stranger, but she was extremely welcoming and she was a nurse, a wellness specialist, and so we had a lovely conversation about this as a choice. I ultimately decided that I was not going to go breast-less but in the meantime, in the middle of all that, I ended up going to a store that sells breast prostheses with my daughter. Before I even knew what I was doing I spent 500 dollars on this thing, which as a reminder to my reactivity now, sits in my dresser drawer.
Elaine: So this is again what you’re saying earlier about letting yourself have a few breaths to make decisions without feeling you have to make a decision right away.
Patricia: Yeah. Like our anxiety, our reactivity, makes us act quickly because, I think what we want is to get away from the discomfort of the emotion not because we actually have to do something. There was no urgency to go buy a silicone breast, it wasn’t necessary. It could have waited — it could have waited a long time.
Elaine: Now there’s something about the story of you going up to that woman on the subway that I also found really tender and interesting because it speaks to actually a really beautiful side of the cancer story, which is the ability to begin to relate to the world in a new way from, dare I almost call it, a community standpoint. I was in a, I feel, privileged position to be on your care team and help organize people to bring you food, for example. And it wasn’t that I had to go and find people, it was more I needed to help organize all of the people who wanted to help and they just needed somebody to coordinate it so they didn’t all fall over each other to do so. I found it really interesting to notice how — we talk about mindfulness and it made me curious about what mindfulness as a community experience is really, it really opened up a new window for being about that notion.
Patricia: So when we get sick, we think it’s only happening to us. But every big change in our life is also happening to those who are close to us to those who we love and who care for us. And this is something that I don’t think is easy for us particularly in Western culture to see. And I think you’re right that there is something that is a real gift to both the person who is sick and to those who would offer care that comes about when we’re open to our need and our vulnerability and our wish for help — others I actually don’t see it as a burden. I think there’s a tendency to be really private and to hide these things as I was talking about with the wig and in fact I know people who’ve had cancer and they didn’t tell anyone — they went through the whole thing really on their own or with one other person. The cancer experience otherwise is exhausting. The treatment is brutal: It goes on and on and on. One’s life becomes a series of appointments and visits to doctors and other health care professionals and people wanting information from you and you wanting information from them and friends and family wanting to know what’s happening and it really can take over your whole life.
I think behaving as if you actually are an island is really a mistake. You’re pointing to how making the cancer experience a community experience is really the next step in one’s mindfulness journey where we are moving from individual knowledge about our personal experience, our sense of self, to enhancing our compassion for others.
Elaine: Before we started our conversation on tape we were having a conversation about how, for many, mindfulness is viewed as an individualistic journey and you had some really interesting insights about that from being on the inside of what it was to be at the center of a very loving and active community who greatly benefited by being able to participate and come to the hospital with you and bring you food. Can you speak to that a bit.
Patricia: I think it’s a relief both to the person with the illness and to those who are close to be able to be of service and to be of assistance in what often is a situation where people feel helpless. There’s literature to support the idea that as health increases, self concern decreases and concern for others increases and also that those people who are of service to others are happier than those who are not.
Elaine: So in a really kind of almost interesting way, illness can provide anybody who we might consider our community a beautiful opportunity to awaken to something tender in themselves and to get to the heart of what mindfulness really is. Mindfulness is not a way to make a better us but a way to bring awareness to how we’re all here together, breathing together. I think sometimes when we’re all well it’s easier to forget that — when we’re just trucking along. Sometimes when one of us get stopped, especially with somebody we care about, it allows us to go, “Oh right we are all in this together and we want to be in this together.”
“Mindfulness is not a way to make a better us but a way to bring awareness to how we’re all here together, breathing together. I think sometimes when we’re all well it’s easier to forget that.”
—Elaine Smookler
Patricia: If we can bring not just awareness but curiosity and compassion to our experience, whatever it is — compassion is defined as wanting to be of assistance to others, to be with their suffering and to be of assistance. If we can bring those two qualities of curiosity and compassion to our practice, it takes us so much further than when we’re just focused on our sense of self.
Elaine: So that thought makes me curious about if there were any aha moments for you along the way as you mingled your experience of being a human being on a cancer journey with that label called Cancer comingled with your experience of many years as a mindful practitioner and teacher. I’d love to know even more how those things started to reveal themselves.
Patricia: Well I think when you have a serious illness it’s really easy to start to have your thinking be pitched into the future about some nightmare that you may be heading toward. So one of the things that I think the practice helped me do was to be able to recognize when that was happening and pull my thoughts back from that to the experience of body: of the body breathing, of sensation, of waking up to the fact that that’s where my thoughts had gone and therefore I have a choice about is this really what I want to think about or do I want to just check in with what’s here right now, whatever that is, and move off of that kind of thinking, which you could argue is a problem solving strategy but it’s not particularly effective, particularly when it’s really kind of bad fantasy. The other thing is that I found it really hard to sit with any consistent regularity and length of time.
Elaine: When you say “sit” you mean like practice meditation on a cushion.
Patricia: Yeah the formal way, so, very brief practices were helpful for checking in regularly with: Oh what’s here right now in thinking what’s here in emotions, what’s here in the body, what am I experiencing right now. “Oh, fatigue is here. OK, and then being able to make a conscious decision that OK maybe you need to rest now or maybe impatience is here or anxiety is here and then being able to recognize what was going on so this is the awareness piece you’re talking about but then being able to really then make an intentional decision about what to do next from a place where there is a bit of space, a bit of perspective-taking.
Elaine: Right, we often will talk about practices like the STOP practice — little pithy practices that are there to remind us to stop in difficult moments, take a breath, and begin to notice what is here right now. What thoughts are showing up, what feel what physical sensations, what thoughts are here. And then and then the “P” of the STOP practice is then potentially, once we are really able to be present to what’s showing up we’re able to proceed with a bit more wisdom. And I find it notable that you know even though you’ve been a practitioner for many many years and we’ve taught many thousands of people, we see that sometimes people come to mindfulness with this idea that if they practice they’re not going to have difficult emotions, they’re going to be calm. I feel that one of the interesting things you and I have discovered is of course we’re still human beings, we’re going to have strong emotional experiences but potentially the mindfulness gives us a way to be able to hold and frame those experiences without it pulling us down the rabbit hole for an extended period of time, so it really speaks to resilience. Is that something that you would say you related to?
Patricia: In recovery: Quick recovery from those reactions. If one expects one isn’t going to have difficult emotions, good luck with that. It’s what you do when they show up that matters: How do you treat yourself, how do you treat other people, what do you do next. Is it helpful or is it harmful?
Elaine: Beautiful, so whether we’re sick or whether we’re well, we find that awareness is still the same companion where we’re trying to understand: “and now what?” and “how can I be with this? and “how can I be with this: ah, cancer is here,” “ah, pain is here,” “ah, chemo is here,” “ah, throwing up is here,” And being with you and just watching you show grace under vomiting.
Patricia: What you’re also speaking to is the tendency to want to avoid difficulty, to want to turn away from it in an effort to escape. In fact when you have something like a cancer diagnosis, escape really is not possible. It is possible in the short term but if you don’t deal with it and manage it it will take over your life and usually ultimately have a bad outcome. It behooves us to turn toward that which we don’t like or that we’re afraid of or that we would rather not face and find a way to build our tolerance and our resilience, as you were pointing to.
Elaine: So do you have tips that have come from this experience for others who may find themselves also going through this journey either themselves or with others who are going through the journey of cancer.
Patricia: I would say reflect on what actions are really essential and what can wait. Make sure that you have a support system if you’re able to tell people and talk about it. I think this helps everyone to normalize what comes for all of us sooner or later as some sort of illness. Enlist people’s help. Really think about what self-care means.
Elaine: Give me some examples of what self-care meant for you.
Patricia: It meant continuing to exercise while I could because women who do aerobic exercise have better outcomes than those who don’t. Not drinking alcohol because it increases recurrence and it increases the risk of breast cancer significantly in all women. Getting massage was important post surgery, having physio.
Elaine: Why was that massage important?
Patricia: Because there is a lot of pain or because there are various muscular and other problems that can come from the surgery. Also go to bed when you need to. For me it was important to also continue to do some work because I really was aware that I didn’t want my whole identity taken up with this.
Elaine: Your children were adults when you got your diagnosis, but I’d love to know if you had any tips for how to talk to family members when you discovered this diagnosis.
Patricia: Tell the truth. I think it’s not my job to rescue others from my illness nor is it other people’s jobs to rescue the other people in their lives from their illnesses. I don’t think we do people a service by not exposing them to life difficulties. My children were very aware of what was going on and they were incredibly helpful, particularly my daughter. It was I think in some ways the hardest for her because she was the most present throughout the whole process, and she’s young. She was 22 at the time and was really remarkable I think it changed our relationship and it shifted it — where I’m still her mother but she really learned what it meant to look after others, and to be compassionate, and to at times feel the burden of that and at times have to cope with the emotional reactions that comes from the unknown. But I think it was good for her to be part of that and to know about it.
Tell the truth. I think it’s not my job to rescue others from my illness nor is it other people’s jobs to rescue the other people in their lives from their illnesses. I don’t think we do people a service by not exposing them to life difficulties.
Elaine: Now there was another family member who played a really interesting role in your journey. I’d love you to talk about that especially because, as you said, it’s so easy when you’re the one with the diagnosis of cancer to have the view of yourself, you know, you’re weak and everybody needs to take care of you, and yet you did something during your diagnosis I’d like you to talk about that relates to one of your family members.
Patricia: This is great because you’re giving me the opportunity to talk about my “BFF,” my grandson. He was not even two at the time and I was looking after him one day a week before I got the diagnosis, and I continued to look after him one day a week through the whole treatment.
Elaine: Even though people said to you “You shouldn’t be looking after your grandson, you should be resting!”.
Patricia: Yeah, that’s what they said. But, what I did was I still looked after him and then I’d get people to come and help me look after him (laughs). But he was a delight and a great support unbeknownst to him. He made it just so much more possible — there were some times when he had to come to the hospital and there were some times when I would take him to his singing classes and I’d be really weak and kind of left him and all of that —
Elaine: So, how is he a great support?
Patricia: Because he’s really open and present and when you’re with a little kid you have to be present — you can’t really be doing other things. When we’re baking or baking, when we’re playing, we’re playing.
Elaine: And was it interesting for you at all that he wasn’t aware that Nana had cancer? Like everyone else in your life was aware but was he aware?
Patricia: He knew.
Elaine: What did that mean to him?
Patricia: I don’t really know what it meant to him. He was involved in it for the whole process — it was a year and a half — so he wasn’t speaking that much in the beginning but he would ask me questions about why I would have the scar I had and why I had to have a new breast. There’s no question that he’s heterosexual, that kid likes breasts.
Elaine: OK that’s another topic another podcast.
Patricia: He noticed because he was still nursing for quite a while with his mom.
Elaine: Great. Well thank you for sharing that with us. So it’s lovely because one of the things that I think you’re speaking to again when we started this podcast we talked about role like the we’re talking about norms of role and the ability that even in a situation like this to let the role move around a little bit so that we don’t get trapped just like we talk about mindfulness — you don’t want to get trapped in one view.
What happens when your view is all about cancer victim, cancer victim cancer victim, instead of realizing that yes absolutely I have a lot of things that I have to deal with, but that’s only one component of who I am: I me, with cancer. I feel that one of the things that I experienced with the with him and you is just that it was fun to see that you were still grandma and you were still able to go and play in the park and do things with him rather than saying “oh no that part, my life is over.” And I thought that was really interesting. So it would be wonderful to know, so you went through this experience and how are you now?
Patricia: I’m good now. One of the things I did when I was in the middle of treatment— this an act of self-care, a bourgeois act of self-care was I’ve always wanted to be on water. So when I was in the middle of treatment I didn’t really know how it was going to go, I told my husband that I wanted to be on water and I want to do it now. So if I’m going to get sick and die I want to be in water and if I’m not going to get sick and die I want to be on water. So we ended up buying a small cottage on leased First Nations land on water and that was a real act of self-care and it was really in many ways a unilateral decision — of course he had to sign the papers as well for the transaction, but what was he going to say, no you didn’t do this?
Elaine: It’s the old framing it: “If I’m going get sick and die, I dare you to trump that.”
Patricia: Right. One could argue I was playing the cancer card, so it was all fine until I didn’t die, and then he got mad about it but we’ve overcome that now. So how am I now?
Elaine: First of all, diagnosis-wise, where are you at?
Patricia: Yeah I’m well, I’m fine now.
Elaine: What does that mean well?
Patricia: Well, I don’t have cancer at this point as far as I know. And I’m back to living my life but really trying to — trying to — take more space to do the things I want to do and to have time up on the water and have time away with my husband and my family and friends.
Elaine: And I notice that you’re also writing — obviously you’re a professional writer, you do lots of writing about mindfulness — but you also have been writing about cancer and I believe mindful.org is going be publishing some of your experiences about your experience going through cancer, which is wonderful because it’ll give us a bit more. It’s hard to explain to a person who hasn’t gone through cancer or how there could be a humorous side but… I have — maybe wanted to say (laughs).
Patricia: Yeah, yeah. You’ve also been through it too so and you and I have —.
Elaine: “It: being I’m also somebody who’s been through cancer.
Patricia: Yeah. And I mean you and I have been able to bring humor to a lot of difficult situations not to mention that. It’s all well and good for us because we’re well now as far as we know. We can’t really speak to what happens when it doesn’t turn out that way because sooner or later we’re all going to be palliative in one form.
Elaine: But I feel it’s important and I mention it because of course when you’ve got to through it yourself it’s a little bit easier to be able to bring humor in and since I had gone through cancer before Pat went through cancer, I did bring my own perspective of it and found that humor and a relative light touch was also very very helpful when there are dark days when you really just feel kind of yucky. To be able to have a sense of humor even about that, it’s not glib, it is just a way to hold the whole situation with a little bit more lightness knowing, as you said to me before Pat, this too shall pass. Everything passes until eventually we do pass one way or the other. And so I feel that all this gives us an opportunity to look at our lives and for some of us it can be really powerful to go through an experience like this because it can be a wakeup call to our precious lives and to — what’s that line from the wild geese “What will you do with your one wild and precious life.”
Patricia: Mary Oliver, it’s one of my favorite lines and I think you’re absolutely right. I think catastrophic illness can be approached with humor. Humor is definitely an ally and also taking the time to reflect on what will you do with your one wild and precious life, because as far as we know, we only get one.